- Business
- October 14, 2025
Healthcare applications are experiencing unprecedented growth, with projections indicating a market valuation of $4,710.54 billion by 2034, growing at a CAGR of 45.1% (Polaris Market Research). As the demand for these applications rises, the healthcare industry is also facing an alarming increase in data breaches. In 2024 alone, there were 720 reported incidents affecting over 180 million individuals, with hacking being the primary cause, as reported by FOX59 news. The United States holds the highest average breach cost, amounting to $9.48 million.
The penalties for violating HIPAA can reach millions, with civil fines for breaches of the Privacy Rule and Security Rule hitting up to $1.5 million annually.
A singular data breach can initiate not only significant financial implications and legal repercussions for your healthcare organization but also regulatory inquiries, damage to your reputation, and a decline in trust from patients and stakeholders.
What if we told you there’s a way to shield your healthcare IT solutions from such threats without delaying your development timeline or exhausting your finances? Indeed, achieving this is feasible with the right technical framework, a solid comprehension of regulatory guidelines, and a proactive security strategy from the outset.
This guide is tailored for healthcare executives assessing app development, CTOs in the process of creating healthcare apps, product managers, and developers. By engaging with this guide, you’ll uncover the technical necessities for HIPAA compliance, a step-by-step development roadmap, cost estimates, timelines, and real-world strategies for implementation.
Key Takeaways
- HIPAA compliance is essential for any healthcare app that deals with PHI; it’s not merely a “best practice.”
- Failure to comply can result in hefty fines and irreversible reputational harm.
- A security-by-design approach is fundamental to HIPAA-compliant development, encompassing encryption, access management, and audit logging.
- Collaborating with developers experienced in HIPAA regulations simplifies processes, speeds up approvals, and guarantees scalability.
- Building user trust is the ultimate return on investment, and HIPAA compliance enhances brand reliability and patient assurance.
- The cost for developing a HIPAA-compliant app can range from $50,000 to $3,000,000 or higher.
What is HIPAA Compliance?
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 is a federal statute that establishes standards for protecting sensitive patient health information (PHI). Its main objective is to ensure patient data’s privacy, security, and availability to authorized individuals only.
HIPAA’s compliance extends beyond healthcare technology, affecting all covered entities—such as medical providers, health plans, and healthcare clearinghouses—as well as their business associates like application developers managing PHI.
HIPAA Compliance Rules: What the Law Actually States
HIPAA mandates a regulatory structure with established rules governing privacy, security, breach notifications, and compliance enforcement. Grasping these requirements is essential for executives and technology leaders in managing risks, formulating strategy, and investing in technology.
Privacy Rule
- Establishes standards for the protection of PHI.
- Grants individuals rights to access their health records.
- Restricts the use and disclosure of PHI to authorized instances.
- Imposes the minimum necessary standard, requiring only the pertinent PHI for each task to be accessed.
Security Rule
- Requires implementing technical safeguards for electronic PHI (ePHI), such as encryption and access controls.
- Mandates the creation of administrative safeguards, including policies, procedures, and training.
- Specifies physical safeguards, like ensuring secure facilities and workstations.
- Distinguishes between required and addressable implementations based on risks.
Breach Notification Rule
- Defines a breach as unauthorized access or disclosure of PHI.
- Requires notifying HHS/OCR for breaches affecting 500+ individuals.
- Mandates media notifications if over 500 individuals in the same state/jurisdiction are impacted.
- Requires reporting to individuals within 60 calendar days of discovery.
- Also requires notifying individuals and the Department of Health and Human Services (HHS) for breaches affecting fewer than 500 individuals.
Enforcement Rule
- Empowers the Office for Civil Rights (OCR) to ensure compliance.
- Establishes procedures for investigating HIPAA Administrative Simplification Rule violations.
- Outlines civil monetary penalties for such violations.
- Sets compliance, investigation, and hearing standards.
- Codified at 45 CFR Part 160, Subparts C, D, and E.
- Fines are scaled based on violation severity and nature.
- Organizations may undergo audits to validate adherence to HIPAA regulations.
- Understanding enforcement is vital for executives planning digital transformations in healthcare, as non-compliance poses financial and reputational risks.
Omnibus Rule
- Extends HIPAA obligations to business associates, making them directly responsible.
- Fortifies breach notification, patient rights, and privacy safeguards.
- Aligns enforcement and penalties with contemporary healthcare and technology practices.
What Apps Need HIPAA Compliance?
Primarily, healthcare applications such as telemedicine, EHR and EMR systems, healthcare communication tools, medical billing and insurance applications, as well as health monitoring and wearable apps require HIPAA compliance.
However, not all healthcare app development initiatives necessitate HIPAA compliance. If your application involves the storage, processing, or transfer of protected health information (PHI), compliance becomes imperative.
Let’s review the leading healthcare app types for which HIPAA compliance is mandatory:
Telemedicine/Telehealth Apps
These platforms facilitate remote consultations, video conferencing, patient monitoring, and virtual care coordination, making it essential to protect patient data both in transit and during storage.
Read further for the cost of developing a telemedicine application!
EHR/EMR Systems
Electronic Health Record (EHR) and Electronic Medical Record (EMR) systems contain extensive PHI, integrated with solutions like patient portals, clinical documentation, and medical charting applications. As such, stringent access controls, audit trails, and encryption mechanisms must be enforced.
Healthcare Communication Apps
Healthcare providers operating within organizations or tied to specific forums can use messaging or collaboration applications to discuss patient care. If PHI is involved, compliance with HIPAA standards is imperative.
Medical Billing & Insurance Apps
Applications handling medical claims, billing, or insurance details must ensure the protection of both financial and health information against unauthorized access.
Health Monitoring & Wearable Apps
Primarily linked to medical devices, these apps track vital signs, activities, or chronic conditions that produce PHI. Therefore, adherence to HIPAA compliance and interoperability standards is a necessity, ensuring encryption and secure data storage.
NOTE: Consumer wellness applications may NOT require HIPAA compliance if they do not share data with covered entities.
Pharmacy & Prescription Apps
This category includes e-prescription tools, medication management systems, pharmacy inventory applications, and prescription refill services, all of which handle prescriptions, medication histories, or pharmacy orders. Thus, these applications must apply stringent privacy standards.
Mental Health Apps
For apps focused on therapy or counseling—such as a mental health assessment tool like Helponymous—the likelihood of collecting and storing sensitive mental health data is significantly higher. Hence, these apps require additional protective measures due to the nature of the data involved.
Laboratory & Diagnostic Apps
Laboratories and imaging centers handle the most critical patient health information, which can be exploited by pharmaceutical companies or research teams. As such, test results from labs, diagnostic imaging, and pathology reports fall under HIPAA regulations, necessitating secure data processing and audit functionalities.
NOTE:
Some healthcare app development categories do not necessitate HIPAA compliance, which include:
- General wellness applications
- Fitness tracker applications, like 6PP featuring Jeff Cavalier
- Dietary applications
- Meditation applications, such as Rosita
- Medical reference libraries
- Symptom checkers without personalized data storage
- General health information websites
However, you must ensure these apps do not share data with healthcare providers or are not marketed as medical tools.
For more clarity, you can consider the following questions:
- Does the app create, receive, maintain, or transmit PHI?
- Is the app utilized by covered entities or business associates?
- Does the app link to EHR systems or healthcare providers?
If YES to any: HIPAA compliance required
Whether you’re embarking on a complete healthcare app development project or overhauling existing systems, if your app collects information related to individuals or organizations connected to the U.S., compliance with HIPAA is essential.
Why HIPAA Compliance Is Essential for Apps
Adhering to HIPAA is crucial for applications that manage Protected Health Information (PHI), as non-compliance can lead to grave legal consequences, financial penalties, a decline in user trust, and issues surrounding patient safety due to data exposure.
As such, safeguarding sensitive medical information in today’s digital landscape is both a legal and ethical necessity.
Let’s examine why compliance is essential for healthcare applications today:
Violating HIPAA rules can result in substantial financial penalties, ranging from thousands to millions of dollars. These penalties vary based on the violation’s severity and intent.
HIPAA’s penalties could fall into tiered categories enforced by the Office for Civil Rights (OCR), including:
- Tier 1: Fines span from $100 to $50,000 per violation for violations occurring despite a lack of knowledge that could not have been reasonably prevented.
- Tier 2: Fines range from $1,000 to $50,000 per violation, depending on whether the organization should have recognized the violation but acted with willful neglect.
- Tier 3: Fines could be $10,000 to $50,000 per violation for willful neglect addressed within 30 days.
- Tier 4: Fines initiate at $50,000 per violation for willful neglect that remains uncorrected within 30 days.
The maximum annual penalty can hit $1.5 million or more for repeated infractions.
Moreover, criminal penalties for HIPAA breaches may also be imposed by OCR, including:
- Wrongful disclosure: Fines up to $50,000 along with a 1-year prison sentence.
- False pretenses: Fines up to $100,000 and a sentence of up to 5 years.
- Intent to sell/transfer PHI: Fines up to $250,000 with a 10-year prison term.
Beyond fines, organizations may also incur significant costs related to reputation damage, litigation, breach recovery, and corrective measures.
Let’s explore some actual enforcement examples:
- Anthem Inc. incurred a $16 million settlement with OCR after experiencing the largest U.S. health data breach, revealing 79 million records in 2018 due to inadequate access controls and encryption.
- Premera Blue Cross had to pay $6.85 million to OCR for failing to implement risk management and audit controls, leading to a data exposure of 10.4 million records in 2020.
- Touchstone Medical Imaging faced a $3 million settlement with OCR for inadequate security measures and failure to establish Business Associate Agreements (BAAs) in 2019.
Why Aim for HIPAA Compliance in Your Healthcare App?
Striving for HIPAA compliance in app development is critical, as it influences patient rights and confidence, serves as a protective measure and strategic asset for providers, and unlocks numerous advantages.
Let’s explore how developing a HIPAA-compliant app benefits all stakeholders involved:
Benefits for Patients
- Patients gain authority over their PHI, protection against identity theft, and the assurance that their data will not be misused.
- Patients can access their medical records within 30 days, request amendments, and manage how their data is shared.
- They have the right to ask providers for explicit privacy notices, seek consent regarding data use, and receive notifications in the event of a breach.
Benefits for Hospitals and Healthcare Providers
- Avoiding costly fines, lawsuits, and reputational damage.
- Achieving operational excellence by adhering to standardized protocols, enhanced incident responses, and reinforced data governance.
- Distinguishing as a secure, trustworthy provider, enabling eligibility for value-based care partnerships.
- Boosting engagement, retention, and long-term loyalty through transparent practices.
Benefits for App Owners
- Gaining the ability to serve hospitals, insurers, and enterprise healthcare providers.
- The “HIPAA-compliant” label offers a trust signal and a competitive advantage, facilitating premium market positioning.
- Fostering long-term viability through a scalable framework that mitigates compliance setbacks while enhancing investor trust.
- Ensuring stability for operations, safeguarding valuations, and supporting future exit prospects.
In summary, HIPAA compliance is a vital enabler of business that minimizes risks, cultivates trust, and ensures sustainable growth in a high-stakes industry.
HIPAA Compliance Checklist for Healthcare App Development
The HIPAA compliance application development checklist encompasses a compliance assessment, legal foundation establishment, team readiness, architectural planning, data management, implementation requirements, infrastructure setup, and testing procedures.
Below is a comprehensive checklist you should follow to successfully develop a HIPAA-compliant app:
1. Pre-Development Phase Checklist
During this stage, conducting a compliance evaluation, establishing the legal framework, and assembling a qualified team to ensure your healthcare app meets HIPAA mandates is crucial. Here’s a pre-development phase checklist:
Compliance Assessment
- Identify all PHI/ePHI your app is expected to handle.
- Determine if your organization qualifies as a covered entity or business associate.
- Map out all data pathways (where PHI is collected, processed, stored, and transmitted).
- Document third-party services granted access to PHI.
Legal Foundation
- Draft Business Associate Agreements (BAAs) with all applicable vendors.
- Devise privacy policies in alignment with the HIPAA Privacy Rule.
- Create contracts for secure data sharing.
- Establish an incident response plan along with breach notification protocols.
Team Preparation
- Designate a HIPAA Security Officer and Privacy Officer.
- Specify compliance responsibilities for team members.
- Schedule HIPAA compliance training for the workforce.
2. HIPAA-Compliant Healthcare App Architecture & Design Phase Checklist
This phase focuses on the creation of security architecture, access controls, and data administration. Below is the architecture & design checklist:
Security Architecture
- Establish security-by-design architecture.
- Implement encryption for both data at rest and data in transit.
- Create authentication and authorization mechanisms.
- Formulate audit logging structures.
- Design backup and disaster recovery strategies.
Access Controls
- Determine a role-based access control (RBAC) framework.
- Design user authentication protocols (MFA and SSO).
- Establish session management and timeout policies.
- Plan for emergency access processes.
Data Management
- Define data retention practices.
- Establish protocols for secure data disposal.
- Create strategies for data minimization.
- Prepare for de-identification/anonymization where necessary.
3. Development Phase Checklist
This stage encompasses all considerations pertaining to technical implementation, infrastructure requirements, and documentation to guarantee the app’s compliance during development. Here’s what to focus on:
Technical Implementation
- Utilize AES-256 encryption for data at rest.
- Employ TLS 1.2 or higher for data in transit.
- Build a robust authentication system (supporting MFA).
- Establish role-based access controls.
- Implement comprehensive audit logging.
- Incorporate automatic session timeouts.
- Create secure API endpoints.
- Apply input validation and sanitization protocols.
Infrastructure
- Select a cloud provider that adheres to HIPAA regulations.
- Execute BAAs with cloud providers.
- Establish secure network architecture.
- Implement intrusion detection/prevention systems.
- Set up security monitoring and alerting mechanisms.
- Configure automated backup solutions.
- Develop disaster recovery procedures.
Also explore our blog on cloud computing in healthcare to understand how this technology can streamline workflow in the industry.
Documentation
- Document overall system architecture and data flows.
- Formulate security policies and procedures.
- Record risk assessments along with mitigation strategies.
- Create user access management protocols.
- Compile an incident response manual.
4. Testing Phase Checklist
This phase revolves around verifying compliance and security protocols implemented earlier in the planning and development stages:
Security Testing
- Conduct thorough vulnerability assessments.
- Execute penetration testing.
- Assess encryption practices.
- Validate access control mechanisms.
- Verify accuracy and completeness of audit logs.
- Examine session timeout functionality.
- Evaluate data backup and recovery routines.
Compliance Testing
- Confirm that all HIPAA Security Rule standards are fulfilled.
- Test breach notification protocols.
- Validate compliance of BAAs with third-party vendors.
- Review and test the incident response strategy.
- Conduct compliance gap analyses.
5. Deployment Phase Checklist
This checklist guides you in preparing for the healthcare app rollout while ensuring HIPAA compliance:
- Conduct a final security assessment.
- Train all users on security requirements.
- Activate security monitoring systems.
- Establish an ongoing auditing schedule.
- Enforce change management protocols.
6. Onboarding and Ongoing Compliance Maintenance Phase Checklist
Post-launch, consider providing your team with training for HIPAA audits and ensuring compliance is maintained. Therefore, ensure the following:
- Facilitate annual HIPAA training sessions.
- Conduct periodic security risk assessments.
- Reassess and update policies yearly.
- Monitor for security incidents.
- Track and investigate anomalies in audit logs.
- Maintain BAAs with all vendors.
- Ensure that software and security patches are up-to-date.
- Maintain documentation of all compliance activities.

How to Create a HIPAA-Compliant App: A Step-by-Step Process
The process for developing a HIPAA-compliant mobile application should encompass an initial evaluation, planning, the design of a security-first architecture, active development, and deployment with compliance scrutiny. Following that, provisions for ongoing maintenance to ensure adherence to HIPAA as requirements evolve should be examined.
Let’s delve into a sequential approach for building HIPAA-compliant applications:
STEP 1: Preliminary Analysis & Planning
- Your first task is to ascertain whether HIPAA is relevant to your healthcare application by identifying whether it processes PHI/ePHI and delineating the organizational type (covered entity or business associate), while also mapping the flow of PHI. For assistance, you may hire data engineers.
- Gather a cross-functional team comprising legal, compliance, security, and engineering members for a comprehensive risk assessment.
- Based on the findings of the risk assessment, compile a list of HIPAA controls required, establish user roles, delineate access permissions, and determine which parts of your system will manage PHI versus non-PHI to implement compartmentalization effectively.
- Select a cloud service provider that offers HIPAA-compliant services and is willing to enter into a Business Associate Agreement (BAA).
STEP 2: Design Security-First App Architecture
- Separate personally identifiable information (PII) from health-related data and substitute it with non-sensitive equivalents such as tokens or surrogate keys. This pseudonymization strategy mitigates risks of data exposure and assists in making the app HIPAA-compliant.
- Establish robust identity and access management with unique user IDs, multifactor authentication (MFA), RBAC, and strong password policies, along with automatic session timeouts and provisions for emergency access in urgent cases.
- Encrypt PHI during both transit and storage, implement integrity controls (HMACs and checksums), and ensure secure key management practices.
- Set up a logging system to capture all access points, changes, and failures, ensuring logs are tamper-resistant and stored securely, along with conformity to HIPAA’s retention requirements.
- Design an architecture that supports regular backups, encryption, a recovery plan, session clearances upon logout, and a remote wipe mechanism for lost devices.
- Employ input validation, sanitize requests, avoid injection attacks, and protect against vulnerabilities typical of healthcare-based web and mobile applications.
- Incorporate API gateways, rate limiting, and authentication tokens while enforcing minimal permissions for each endpoint.
- Minimize PHI exposure within logs, push notifications, debugging windows, or user interfaces, applying de-identification/anonymization where full identity is unnecessary.
STEP 3: Develop HIPAA-Compliant Apps
- Engage mobile app developers who adhere to secure coding standards during app development, emphasizing code review, analysis, linter/security scanning, vulnerability assessment, and frequent updates.
- Separate development, staging, and production environments while steering clear of PHI in non-production settings (using synthetic data where appropriate) and limiting access to those environments while documenting changes.
STEP 4: Test HIPAA Compliant Apps
- Test encryption, access controls, and logging mechanisms to confirm they function as intended.
- Conduct both external and internal penetration testing to identify potential threats, address them, and validate remediation.
STEP 5: Deployment & Compliance Verification
- Review the completed healthcare app and supporting documentation with legal/compliance authorities, making necessary adjustments if any discrepancies arise during deployment.
- Ensure that every external service managing PHI is governed by a properly structured BAA.
- Conduct an internal or external audit concerning HIPAA requirements and remediate any gaps uncovered before fully launching.
- Incorporate all policies, protocols, access rules, and incident escalation pathways to confidently initiate your deployment.
- Deploy the final product with requisite logging, alerting, and monitoring systems activated.
STEP 6: Post-Launch & Ongoing Maintenance
- Periodically reassess threats, identify new vulnerabilities, monitor changes within the technology stack or third-party services, and update the risk register, remediation strategies, and compliance roadmap.
- Review the implications of new features or changes to ensure they align with HIPAA standards.
- Swiftly apply necessary security patches to the operating system, libraries, frameworks, and dependencies.
- Regularly refresh policies, documentation, and staff training especially when policies or technologies are altered.
- Reassess vendor compliance, renew or revise BAAs, and excise or replace non-compliant vendors as needed.
What Safeguards To Consider In HIPAA Compliant App Development Process
In developing a HIPAA-compliant healthcare application, adherence to three primary safeguards is crucial: physical, technical, and administrative.
These safeguards are security protocols mandated by the HIPAA Security Rule to protect electronic protected health information (ePHI).
Here’s an overview of the requirements set forth by HIPAA safeguards:
Administrative Safeguards
These comprise policies and protocols that govern how an organization safeguards ePHI. The administrative safeguards include:
- Policies designed for assessing risks and implementing security measures.
- Designating responsibility for security.
- Training staff in security policies and practices.
- Procedures dictating access to ePHI.
- Backup and disaster recovery strategies.
- Regular assessments of the effectiveness and implementation of security measures.
Physical Safeguards
These are tangible measures to shield facilities and equipment from physical threats or unauthorized access. Physical safeguards foster:
- The restriction of physical access within facilities housing ePHI.
- Securing workstations that access ePHI.
- Developing procedures for the disposal and reuse of electronic media containing ePHI.
Technical Safeguards
These are the technological controls designed to safeguard electronic health information. Technical safeguards stipulate:
- Implementing measures, like unique user IDs, to regulate access to ePHI.
- Establishing audit controls for systems recording and assessing activities involving ePHI.
- Ensuring data integrity by suggesting controls to protect ePHI from inappropriate alteration or destruction.
- Verifying the identities of individuals or entities accessing ePHI.
- Employing measures like encryption to safeguard ePHI during its transmission.
Key Features of a HIPAA-Compliant App
Essential features of a HIPAA-compliant application encompass user authentication, role-based access management, secure messaging, consent management, audit trails, data backup and recovery plans, automatic session termination, and a breach notification system.
Let’s delve into the key features a HIPAA-compliant application should include:
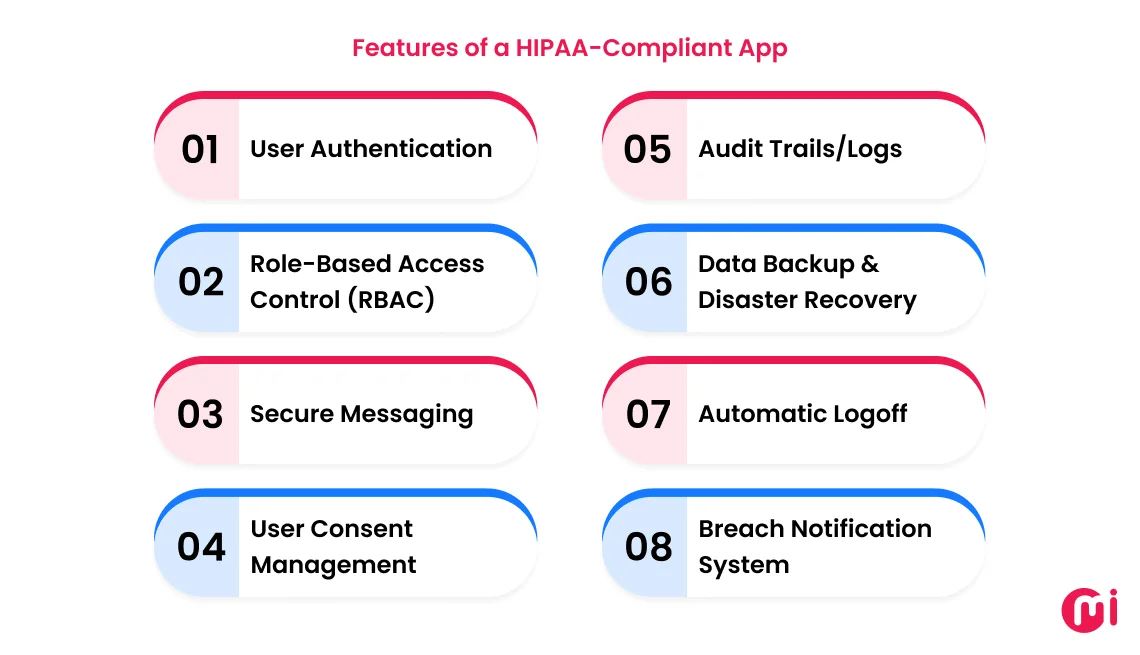
1. User Authentication
A robust user authentication system, employing unique usernames, stringent password protocols, multi-factor authentication, or biometric features is crucial to ensure that only authorized personnel gain access to the app.
2. Role-Based Access Control (RBAC)
This RBAC functionality clarifies access permissions based on roles and requirements. For instance, doctors should have comprehensive access to patient health histories, whereas hospital accounting staff may not need the same level of access. This feature is designed to avert unauthorized data access.
3. Secure Messaging
Secure messaging functionality enables users to interact within the app in a safe manner. By encrypting messages, the app ensures the protection of sensitive health information from interception or unauthorized access, facilitating reliable and private communication between patients and providers.
4. User Consent Management
Consent management enables users to determine how their data is collected, utilized, and shared. Adequate consent tracking ensures transparency while keeping your app compliant with HIPAA privacy stipulations.
5. Audit Trails/Logs
Maintaining comprehensive audit logs of user actions, data access, and modifications is imperative for monitoring compliance, detecting potential breaches, and ensuring accountability throughout the application.
6. Data Backup & Disaster Recovery
Regular backups and a comprehensive disaster recovery strategy safeguard PHI against data loss, system failures, or cyber threats. Ensuring rapid restoration of critical data promotes the app’s reliability.
7. Automatic Logoff
Automatic logoff functions terminate sessions following periods of inactivity, shielding sensitive information from unauthorized access if a device is left unattended.
8. Breach Notification System
A breach notification mechanism ensures that any data security incidents are swiftly detected and reported to affected users and authorities, ensuring the app’s compliance while maintaining user confidence.
Explore our blog on AI in healthcare to discover how to leverage this transformative technology for favorable results.
Cost to Develop a HIPAA-Compliant App
The cost associated with HIPAA-compliant app development typically ranges from $50,000 to $3,000,000 or more.
This cost fluctuates based on factors such as the app’s complexity, features, integrations with third-party services, geographical location, developer expertise, quality assurance, audits, and security compliance implementations.
Let’s break down the costs associated with HIPAA app development based on complexity:
| Complexity Type | Typical Features | Cost Range |
| Basic or MVP Solution | – User authentication – Appointment scheduling – Basic messaging, etc. |
$50,000 – $100,000 |
| Mid-complexity | – EHR/EMR integrations – Secure messaging – Telehealth – Dashboards |
$100,000 – $250,000 |
| Advanced or Enterprise-grade Healthcare App | – Bi-directional EHR – Real-time data sync – AI integration – Wearable integration – Large scale |
$250,000 – $500,000+ |
Mistakes That Hinder HIPAA Compliance and Corresponding Best Practices
Common pitfalls include inadequate employee training, ineffective risk assessments, and lax data security. However, these can be addressed through forward-thinking strategizing and the utilization of automated tools powered by AI.
Perceiving Compliance as a “One-Off Task”
Many healthcare decision-makers mistakenly believe that HIPAA compliance concludes when an app is launched. Conversely, continuous updates of policies, audits, and risk assessments are required to ensure compliance remains intact.
Best Practice: Establish a continuous compliance procedure that includes quarterly risk evaluations, automated monitoring, and routine documentation updates.
PHI Storage in Non-Compliant Environments
In their drive to create feature-rich healthcare applications, teams often neglect the critical step of signing Business Associate Agreements (BAAs) with third-party APIs, CRMs, or cloud service providers.
A frequent oversight during rapid development is inadvertently allowing PHI to be stored in cloud regions outside approved juristic areas, which could instantly render your application non-compliant with HIPAA.
Best Practice: Rely solely on HIPAA-compliant cloud services (e.g., AWS, Azure, and Google Cloud) and ensure each vendor that handles PHI is covered by a signed Business Associate Agreement (BAA).
Discover how healthcare organizations benefit from the Google Cloud in our blog post.
Insufficient Access Controls and Authentication
Healthcare decision-makers often overlook the necessity of enforcing strong password protocols. Consequently, developers may design healthcare applications that allow shared access, weak passwords, or lack multifactor authentication, increasing the likelihood of PHI exposure.
Best Practice: Implement RBAC, enforce multifactor authentication, and ensure that all access logs remain auditable for the required six years, as set by HIPAA’s retention rule.
Neglecting Administrative Safeguards
When aligning a healthcare app with HIPAA standards, training and the establishment of internal policies may often be overlooked. Lack of HIPAA knowledge among employees can leave vulnerabilities that may lead to breaches or information leaks.
Best Practice: Provide employee training on PHI management, define escalation pathways for breaches, and clearly delineate administrative responsibilities.
Vendor and Third-Party Compliance Oversight
Healthcare organizations typically collaborate with HIPAA-certified vendors. However, without thorough documentation or audit trails, these certifications may become meaningless.
Best Practice: Conduct vendor due diligence and request proof of HIPAA compliance, including audit logs and certification reports prior to integration.
Inadequate Documentation and Audit Preparation
Frequently, healthcare organizations fail to formulate adequate documentation, often lacking comprehensive privacy policies, incomplete logs, or no incident response protocol. Such mistakes may lead to failure during a HIPAA audit, even if the application is technically secure.
Best Practice: Generate centralized compliance documentation that addresses all necessary elements, including privacy policies, Business Associate Agreements (BAAs), and breach response strategies. This ensures that your organization can clearly demonstrate accountability and readiness during audits.
Ready to Develop Your HIPAA-Compliant App with MindInventory?
Developing a HIPAA-compliant mobile application solution goes beyond just coding; it entails securing patient information, ensuring efficient workflows, and achieving audit readiness.
At MindInventory, we are dedicated to delivering healthcare software development services to create functional and intuitive solutions.
Whether it’s a HIPAA-compliant practice management system or a straightforward telehealth application, we possess the skills and experience to develop secure health applications.
Our adherence to certifications and compliance, such as HIPAA, SOC 2 Type II, and ISO 27001, allows us to execute this process systematically.
So, you may wonder, “how do we ensure an app is HIPAA-compliant?” Our process encompasses:
- Crafting a security-first architecture with encryption, secure storage, and APIs, which protect PHI while at rest and during transit.
- Establishing role-based access controls (RBAC) alongside multifactor authentication.
- From Business Associate Agreements (BAAs) to privacy policies and incident response frameworks, we maintain a centralized documentation system to facilitate seamless audits.
- We meticulously select HIPAA-compliant cloud service providers and third-party services, verifying all agreements to prevent unintended data exposure. Our case study detailing a HIPAA-compliant, cloud-based healthcare solution exemplifies this.
- We implement monitoring, logging, and reporting systems to ensure ongoing compliance as your app grows.
- Whether it’s a patient-doctor consultation platform or real-time health monitoring, our applications utilize encrypted channels coupled with intelligent consent management to protect sensitive data.
- We ensure compliance does not compromise usability. Patients, providers, and administrators enjoy a seamless user experience while remaining fully secure through our senior-led UI/UX design services.
FAQs About HIPAA-Compliant App Development
What occurs if the app fails to comply with HIPAA?
Neglecting HIPAA compliance in your healthcare application could result in far-reaching consequences including substantial financial penalties, loss of trust, negative media coverage, heightened liabilities, legal actions, subdued growth, and compromised partnerships.
Is a BAA (Business Associate Agreement) necessary when creating a HIPAA-compliant app?
Yes, a Business Associate Agreement (BAA) is essential when developing a HIPAA-compliant app if any third-party vendors or service providers can access PHI by storing or processing data on behalf of your app.
What distinguishes ePHI from PHI?
ePHI refers specifically to Protected Health Information in electronic form, whereas PHI encompasses any identifiable health information, regardless of whether it is in physical or digital format.
What are typical HIPAA violations, and how can they be avoided?
Typical HIPAA violations may include unauthorized access or sharing of Protected Health Information (PHI), such as disclosure without consent, improper handling of records, and lack of security for electronic devices or communications.
To mitigate these violations, organizations should conduct routine risk assessments, provide comprehensive employee training on privacy protocols, implement robust technical safeguards like encryption and access controls, ensure proper record disposal, secure devices, and maintain transparent policies for accessing and sharing PHI.
What transpires during an OCR audit?
During an OCR audit, auditors evaluate documentation, conduct staff interviews, and review security protocols and facilities to detect compliance discrepancies. If non-compliance is detected, the organization must develop a corrective action plan within 60 days to address identified shortcomings.
How much time is needed to develop a HIPAA-compliant app?
Creating a HIPAA-compliant app could take several months to over a year. The overall timeline may extend depending on the project complexity, scope, technologies employed, and the experience level of the development team.
Do international healthcare applications require HIPAA compliance?
No, international healthcare applications do not generally need to adhere to HIPAA unless they manage U.S. patient data or are utilized by U.S. Covered Entities.
How does HIPAA differ from HITECH?
HIPAA establishes the foundational rules for protecting health information and ensuring patient privacy, while HITECH encourages the adoption of digital health information and tightening of HIPAA enforcement.
What challenges arise while making an app HIPAA-compliant?
Healthcare teams often face challenges in interpreting complex regulations, implementing robust encryption and access controls, and maintaining meticulous audit logs. Effectively managing secure third-party integrations while adhering to BAAs, and staying updated with ever-evolving compliance standards can become daunting. Additionally, balancing stringent security measures with delivering a smooth user experience presents another significant challenge.