Blue Cross Blue Shield of Massachusetts is implementing a new program that utilizes a computer algorithm to analyze doctors who frequently bill the insurer for costly patient visits. The insurer aims to identify and reduce payments to physicians who are deemed to have overcharged for their services, targeting what it refers to as outliers in the medical community. This initiative is set to be launched around Nov. 3 as a response to the escalating healthcare costs that have been on the rise for more than two decades, affecting the 3 million members of the insurance provider.
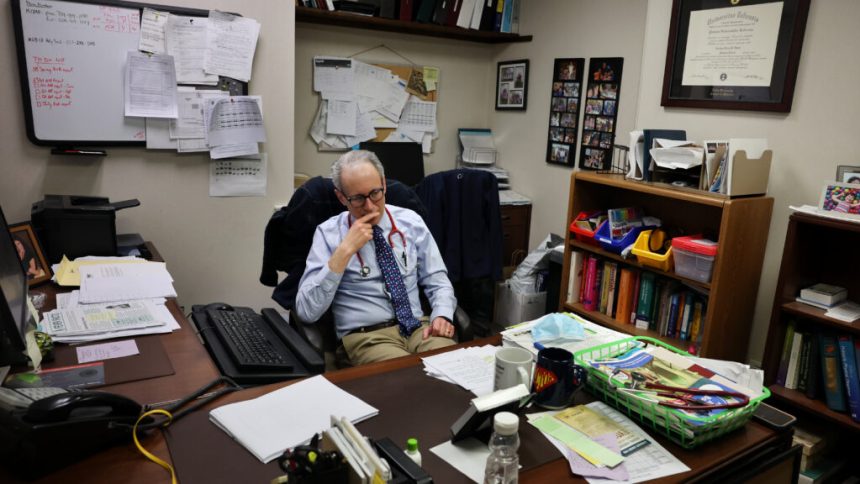
However, this move has sparked criticism from some healthcare providers, especially those who specialize in treating older patients with complex medical conditions. These doctors argue that Blue Cross’s algorithm fails to acknowledge the inherent variability in patient care and treatment plans, which cannot always be neatly categorized by insurance companies and software developers. They emphasize the importance of individualized care tailored to each patient’s unique needs, rather than basing reimbursement decisions solely on quantitative data.
The debate around Blue Cross’s new program underscores the ongoing tension between cost containment measures in healthcare and the delivery of high-quality, patient-centered care. While insurers seek to curb expenses and ensure financial sustainability, healthcare providers advocate for a more holistic approach that prioritizes patient well-being and clinical judgment.
As the healthcare industry continues to evolve, finding a balance between cost-effective practices and personalized care remains a central challenge. It is crucial for stakeholders to engage in open dialogue and collaboration to address these complex issues and ensure that patients receive the best possible care without compromising financial viability.