These genes are kept in check by the immune system, which recognises and eliminates abnormal cells before they can form tumours. With a more diverse and robust immune system, women are better equipped to detect and destroy these rogue cells, giving them a lower risk of developing cancer.
Furthermore, the immune system’s ability to remember past infections and mount a rapid response upon re-exposure is crucial for long-term immunity. This memory function is governed by immune cells called memory T cells, which are more abundant and efficient in women than in men. This means that women are not only better at fighting off infections initially but also at preventing them from recurring in the future.
Another key player in women’s immune advantage is the hormone estrogen. This hormone plays a significant role in modulating immune responses, enhancing the production of antibodies and activating immune cells to combat pathogens. Estrogen also helps regulate inflammation, a critical process in the immune response that, when dysregulated, can lead to chronic diseases such as autoimmune disorders.
Women’s immune systems also age more gracefully than men’s, with studies showing that women maintain higher levels of immune function well into old age. This resilience may be attributed to the protective effects of estrogen, which helps preserve the integrity of immune cells and tissues over time.
Harnessing the power of the female immune system
The emerging understanding of women’s immune superiority has far-reaching implications for healthcare and disease prevention. By tailoring treatments and interventions to account for sex-based differences in immune function, healthcare providers can improve outcomes and reduce the burden of disease in both women and men.
For example, cancer therapies could be optimised to leverage women’s natural immunity and enhance the body’s ability to target and destroy cancer cells. Vaccination protocols may also be adjusted to maximise the effectiveness of vaccines in women, who tend to generate stronger and more durable immune responses than men.
Furthermore, the insights gained from studying women’s immune systems could inform the development of novel treatments for a variety of infectious diseases, autoimmune disorders and chronic conditions. By capitalising on the unique strengths of the female immune system, researchers and healthcare professionals can revolutionise the way we approach healthcare and disease management.
In conclusion, the female immune advantage is a testament to the remarkable complexity and adaptability of the human body. By unlocking the secrets of women’s immune strength, we have the opportunity to revolutionise healthcare and usher in a new era of personalised medicine that benefits all individuals, regardless of gender. As we continue to unravel the mysteries of the immune system, one thing is clear: women are leading the way in the fight against disease, and their resilience and fortitude will shape the future of healthcare for generations to come.
The differences between male and female immune systems have long been a topic of interest in the scientific community. Recent research has shed light on how genetics, hormones, and cellular mechanisms play a role in shaping these disparities.
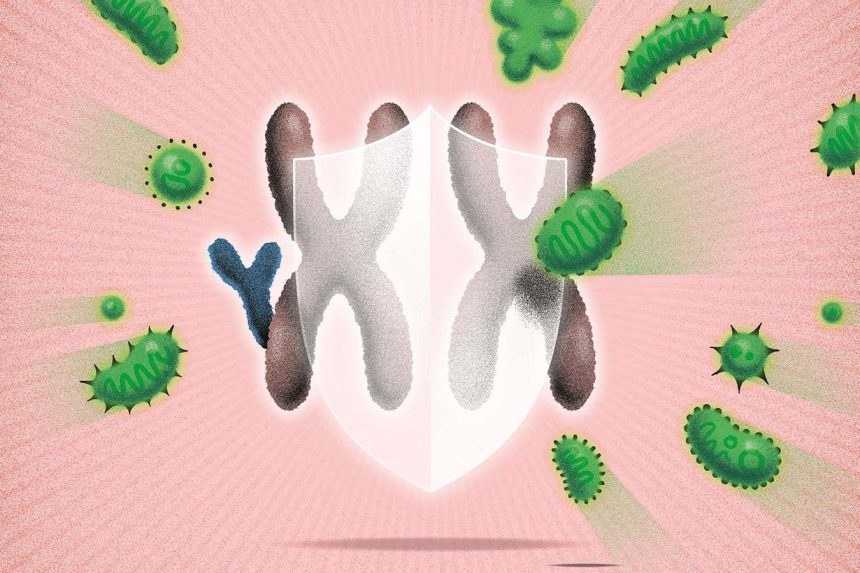
Some genes responsible for immune function are located on the X chromosome, giving women a backup copy that can override errors when things go wrong. This redundancy provided by two X chromosomes could potentially explain why female brains show greater resilience in aging. On the other hand, the Y chromosome, once considered a genetic wasteland, has been found to influence immunity in men, sometimes in detrimental ways. For example, a lineage of the Y chromosome common in men of European descent increases their risk of coronary artery disease due to elevated inflammation and a suppressed immune response.
Studies have shown that women have a lifetime advantage when it comes to immunity, as they are less likely to acquire infections in hospital settings compared to men. This advantage is attributed to fundamental genetics, with women consistently showing stronger immune responses to viral triggers.
Hormones, particularly estrogen, also play a crucial role in shaping the female immune system. Estrogen enhances both innate and adaptive immunity by modulating immune cell activity, leading to a faster and more precise immune response. Neutrophils, a type of white blood cell, are more sensitive to invaders in women due to estrogen activation, making them better equipped to detect and destroy pathogens.
Furthermore, estrogen influences the development of B-cells, which produce antibodies to neutralize invaders. Women’s immune systems run more cycles of refinement in antibody production, resulting in tighter-fitting antibodies and more effective immune responses. Memory B-cells, responsible for storing past pathogen encounters, are retained longer in females across various species, potentially explaining why women have stronger and more durable responses to vaccines.
Research has also shown that women maintain superior B-cell function even after menopause, which may contribute to their longer-lasting immune strength compared to men. As individuals age, men experience a more significant decline in immune capacity in their early 60s compared to women, potentially explaining why older men are more susceptible to infectious diseases.
However, a more reactive immune system in women can sometimes lead to autoimmune diseases, as women are more prone to developing these conditions compared to men. The interplay between genes and hormones likely underlies this susceptibility to autoimmune diseases in women.
Overall, the intricate interplay of genetics, hormones, and cellular mechanisms contributes to the differences in immune responses between men and women, highlighting the complexity of the human immune system. The phrase “it’s a double-edged sword” perfectly encapsulates the complex relationship between the immune systems of men and women. While both sexes face unique challenges and advantages when it comes to fighting off illnesses, the differences between male and female immune responses are often overlooked in medical research and treatment protocols.
One of the key differences lies in the impact of sex hormones on the immune system. Women experience fluctuating hormone levels throughout their lives, which can significantly influence their immune responses. For example, estrogen boosts many aspects of female immune function, while testosterone can suppress immune cell activity in males. This hormonal influence plays a crucial role in how men and women respond to infections, vaccines, and cancer treatments.
In medical research, lumping data from male and female participants together can lead to skewed results and inappropriate treatments. Sex-specific reactions can get averaged out, resulting in men receiving inadequate doses of medication and women being overmedicated. This one-size-fits-all approach fails to account for the nuanced differences in immune responses between the sexes, leading to suboptimal outcomes for patients.
For example, in cancer treatment, understanding how sex hormones influence responses to different therapies is essential. Researchers are exploring how to leverage hormones to maximize immune responses to cancer treatments, potentially leading to more effective and personalized therapies. Similarly, individuals with long covid or ME/CFS may benefit from tailored treatments that consider their unique immune profiles, such as the use of diabetes drug metformin to lower reactive oxygen species levels in women with these conditions.
By acknowledging and studying the immunological differences between men and women, researchers can develop more targeted and effective treatments for a range of health conditions. Understanding how female bodies fight illness and adapt to health challenges can lead to better vaccines, fewer autoimmune flare-ups, and improved outcomes for patients. It’s time for medicine to recognize that strength isn’t just about brute force—it’s about adaptability, endurance, and intelligence in the face of health challenges. And that requires a deeper understanding of the unique immune responses of both men and women. Testosterone is often associated with male characteristics such as muscle mass and aggression, but recent research has shown that this hormone also plays a significant role in shaping immunity. Understanding how testosterone affects the immune system could lead to more tailored medical treatments, including vaccine dosing, that better support the needs of both men and women.
Studies have shown that testosterone can have both positive and negative effects on the immune system. On one hand, testosterone has been found to enhance certain immune responses, such as the production of antibodies in response to infections. This can be beneficial in fighting off pathogens and preventing illness. However, high levels of testosterone have also been associated with a suppressed immune response in some cases, making individuals more susceptible to certain diseases.
One area where understanding the role of testosterone in immunity could have a significant impact is in vaccine dosing. Research has shown that men and women may respond differently to vaccines, with women often mounting a stronger immune response. By taking into account the influence of testosterone on immunity, healthcare providers could potentially adjust vaccine dosages to ensure that both men and women receive the optimal level of protection.
Additionally, a better understanding of how testosterone shapes immunity could lead to more personalized medical treatments for a range of conditions. For example, certain autoimmune diseases, such as lupus and rheumatoid arthritis, are more common in women than men. By considering the impact of testosterone on immune function, healthcare providers may be able to develop more effective treatments that take into account the unique immune profiles of male and female patients.
Overall, the research on testosterone and immunity highlights the importance of considering sex differences in medical treatment. By tailoring treatments to account for the influence of testosterone on immune function, healthcare providers can ensure that both men and women receive the care they need to stay healthy. As our understanding of testosterone and immunity continues to evolve, we can expect to see more personalized and effective medical interventions that support the diverse needs of patients. The world of technology is constantly evolving, with new innovations and advancements being made on a regular basis. One of the most exciting developments in recent years is the rise of artificial intelligence (AI), which is revolutionizing the way we live and work. AI is a branch of computer science that aims to create machines that can perform tasks that normally require human intelligence, such as learning, reasoning, problem-solving, and understanding natural language.
One of the key areas where AI is having a significant impact is in the field of healthcare. AI has the potential to revolutionize the way we diagnose and treat diseases, making healthcare more efficient, accurate, and accessible. For example, AI-powered algorithms can analyze medical images, such as X-rays and MRIs, to detect abnormalities and help doctors make more accurate diagnoses. This can lead to earlier detection of diseases, which can significantly improve patient outcomes.
AI is also being used to develop personalized treatment plans for patients. By analyzing data from electronic health records, genetic information, and other sources, AI can help doctors tailor treatment plans to individual patients, taking into account factors such as age, gender, medical history, and lifestyle. This can lead to more effective treatments and better outcomes for patients.
In addition to diagnosis and treatment, AI is also being used to improve the efficiency of healthcare systems. For example, AI-powered chatbots can help patients schedule appointments, refill prescriptions, and get answers to medical questions, reducing the burden on healthcare providers and improving patient satisfaction. AI can also help hospitals optimize their operations, such as by predicting patient admissions and staffing levels, improving resource allocation and reducing wait times.
Overall, AI has the potential to transform the healthcare industry, making it more efficient, accurate, and accessible. However, there are also challenges and concerns associated with the use of AI in healthcare. For example, there are ethical and privacy concerns related to the use of AI to analyze sensitive patient data. There are also concerns about the potential for AI to replace human healthcare providers, leading to job losses and a loss of human touch in patient care.
Despite these challenges, the potential benefits of AI in healthcare are too great to ignore. By harnessing the power of AI, we can improve patient outcomes, reduce healthcare costs, and make healthcare more accessible to people around the world. As AI continues to advance, it is clear that the future of healthcare will be shaped by this powerful technology.