This groundbreaking achievement involved the correction of a mutation that caused a genetic disorder called hereditary transthyretin amyloidosis (ATTR), a condition that affects the nervous system and heart. Using base editing, the team was able to successfully edit the DNA in the liver of a patient with this rare disease, marking a significant milestone in the field of gene therapy.
Another milestone was the first successful editing of a mutation in a patient with sickle cell disease. By using base editing technology, researchers were able to correct the mutation that causes this debilitating blood disorder, offering hope for a potential cure for this condition.
These successes in clinical trials highlight the potential of base editing and other gene editing technologies to revolutionize the treatment of genetic diseases. As more trials are conducted and more data is gathered, scientists are optimistic about the future of personalized medicine and the ability to tailor treatments to individual patients based on their unique genetic makeup.
Challenges and Opportunities Ahead
Despite these remarkable achievements, there are still challenges to be overcome in the field of gene editing. One of the major hurdles is the off-target effects of gene editing technologies, which can lead to unintended changes in the genome and potential long-term consequences.
Researchers are working on improving the specificity and accuracy of gene editing tools to minimize off-target effects and ensure the safety of these therapies. Advances in technology and a better understanding of the underlying mechanisms of gene editing are helping scientists address these challenges and move closer to the goal of safe and effective gene therapies.
As the field of gene editing continues to evolve, the possibilities for personalized medicine are endless. With the ability to precisely edit the genetic code, researchers are exploring new avenues for treating a wide range of genetic diseases and disorders, offering hope for patients who previously had limited treatment options.
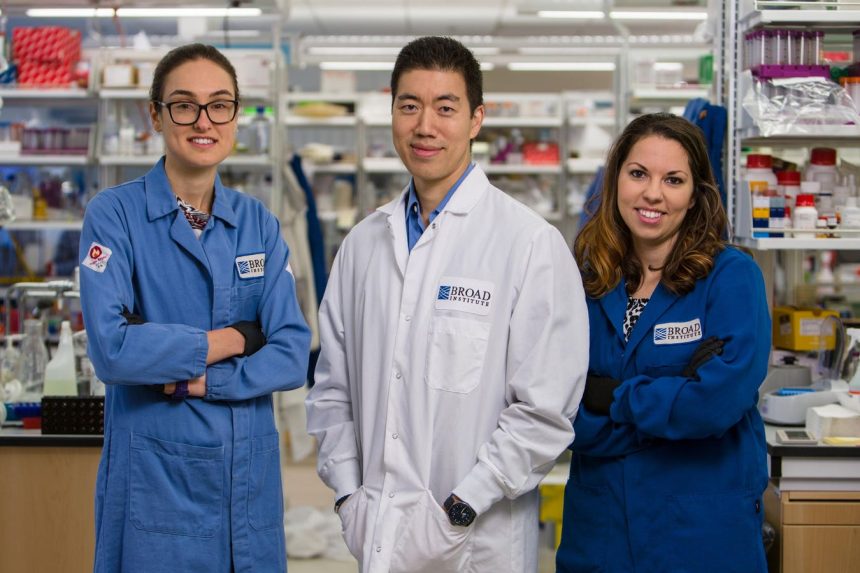
Dr. David Liu and his colleagues at the Broad Institute are at the forefront of this exciting research, pushing the boundaries of what is possible in gene editing and personalized medicine. Their work with baby KJ Muldoon and other groundbreaking clinical trials are paving the way for a future where genetic diseases can be treated with precision and efficacy.
As we look ahead to the next chapter in gene editing and personalized medicine, it is clear that the potential for transformative therapies is within reach. With continued innovation and collaboration, the possibilities for improving the lives of patients with genetic diseases are limitless.
Scientists at Beam Therapeutics, co-founded by Liu, have made groundbreaking advancements in gene editing technology. One of their recent achievements was correcting the most common mutation that causes alpha-1 antitrypsin deficiency (AATD) using a base editor. This development has significant implications for treating genetic diseases.
The potential of base editing combined with a delivery vehicle like an adeno-associated virus (AAV) opens up possibilities for addressing multi-systemic diseases. These diseases affect multiple tissue types in the body, requiring edits in various areas to improve patient outcomes. For instance, in the case of baby KJ who suffered from a liver disease, the base editor was delivered via a lipid nanoparticle specifically targeting the liver to alleviate symptoms.
Liu is particularly enthusiastic about using base editing to treat patients with progeria, a condition characterized by rapid aging. The disease stems from a mutation in the LMNA gene, leading to the production of a faulty protein that damages cell nuclei. Given that progeria affects multiple tissues throughout the body, the ability of base editing therapy to reach different areas is crucial for effective treatment.
Moreover, the development of prime editing, a more versatile tool for correcting DNA alterations, complements base editing in addressing a wide range of genetic mutations. Together, base and prime editing techniques can target over 90% of known disease-causing mutations.
The first prime editing clinical trial yielded promising results in patients with chronic granulomatous disease. This rare immune disorder was treated with a prime editing therapy that successfully inserted missing genetic material, resulting in functional immune cells. The success of this trial marks a significant milestone in therapeutic genome editing.
Looking ahead, Liu envisions a future where base and prime editing therapies could be used for disease prevention. By effectively treating genetic disorders, these technologies have the potential to reshape medicine and empower individuals to take control of their genetic destinies. While gene editing may not eradicate all diseases overnight, the progress made by Liu and his team paves the way for a revolutionary shift in healthcare.
In conclusion, the advancements in base and prime editing technologies offer hope for patients with genetic diseases and lay the groundwork for a new era in medicine. With ongoing developments and advancements in gene editing, DNA may no longer be seen as an unchangeable fate, but rather a malleable blueprint for personalized healthcare.