Philadelphia Hospitals Make Groundbreaking Decision to Stop Using Race-Adjusted Algorithms
A significant development in healthcare was announced yesterday as a coalition of 12 Philadelphia-area health systems declared their decision to discontinue the use of race adjustments in four commonly used clinical tools. This move is expected to enhance treatment outcomes and reduce delays in diagnosis for Black, Hispanic, and Asian patients. The inclusion of race in these tools has been a subject of controversy since 2020, with many clinicians pointing out the flawed science behind depicting race as biological and the potential harm it can cause to marginalized patients.
The initiative in Philadelphia began last year when Seun Ross, a family nurse practitioner and executive director of health equity at Independence Blue Cross, recognized the need to eliminate outdated notions of race from clinical tools. This decision reflects a broader trend in the healthcare industry to address issues of bias and inequality in medical practices.
Provider Identifier System Adds Gender Options, but Uptake Remains Low
In a recent study published in JAMA, it was revealed that out of nearly 127,000 clinicians who registered for their identifier with new gender options, only 0.7% selected the additional choices of “unspecified or another gender identity” and “undisclosed.” This data highlights the challenges faced by healthcare providers in embracing diverse gender identities and the impact of policy environments on their decisions.
The study also found that clinicians in states with negative gender policy environments were less likely to choose these new gender options, underscoring the influence of legislative barriers on healthcare practices. This study sheds light on the importance of creating inclusive environments for healthcare providers and patients of all gender identities.
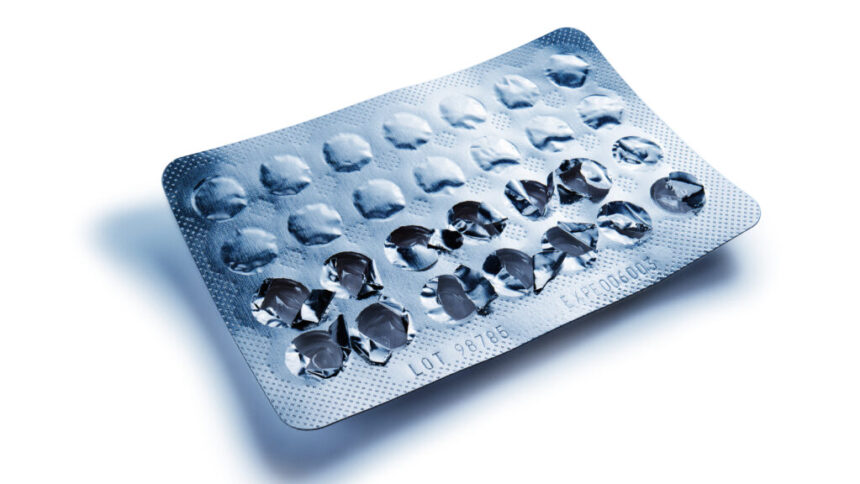
White House Proposes Free Over-the-Counter Birth Control
In a significant policy proposal, the White House introduced new rules requiring most health insurers to cover the cost of over-the-counter contraceptives such as birth control pills, condoms, and Plan B. The proposed rule aims to expand access to a wider range of birth control options and reduce barriers to reproductive healthcare for individuals across the country.
According to experts, the implementation of this rule is not expected to incur significant costs for insurers, as competition in the contraceptive market could lower individual costs over time. This proposal aligns with efforts to improve access to reproductive care and has been a key focus of Vice President Kamala Harris’s campaign.
Global Cholera Cases Decline, but Deaths Spike in 2024
Recent data from the World Health Organization (WHO) revealed a 16% decrease in cholera cases worldwide compared to the previous year, but a concerning 126% increase in deaths. The spike in deaths is attributed to outbreaks in areas affected by conflict, flooding, and limited access to healthcare facilities, with countries like Afghanistan, Sudan, the Democratic Republic of the Congo, and Nigeria being particularly impacted.
Additionally, WHO reported that the global stockpile of cholera vaccine has been depleted, highlighting the urgent need for replenishment to address ongoing outbreaks. The rise in cholera-related deaths underscores the importance of strengthening healthcare infrastructure in vulnerable regions to prevent future crises.
Debate Arises Over Primary Care Physicians Performing Abortions
In a thought-provoking essay, a family physician and OB/GYN advocate for primary care physicians (PCPs) to play a more significant role in providing abortion care. While PCPs currently account for a considerable percentage of abortion providers in the U.S., there is ongoing debate about expanding their involvement in this area of healthcare.
Research indicates that PCPs can offer safe and effective abortion care, potentially reducing the need for patients to travel out of state for services. The discussion around PCPs performing abortions raises important questions about expanding access to comprehensive reproductive healthcare and the role of primary care providers in addressing patients’ diverse needs.
Source: Stat News