Current Heart Attack Screening Techniques May Miss Half of Those at Risk, Study Finds
A recent study has revealed that existing medical screening methods might be failing to identify almost half of individuals who are at risk of experiencing a heart attack. This research suggests that by enhancing screening techniques, many of the millions of heart attacks that occur annually could potentially be prevented.
In the United States, the assessment of heart attack risk typically involves evaluating criteria such as the atherosclerotic cardiovascular disease (ASCVD) score, which considers factors associated with cardiovascular disease development. Patients are then monitored or treated based on whether their scores surpass a certain threshold.
A team of researchers from the US and Canada examined the health records of 465 individuals aged 65 or younger who had experienced their first heart attack between January 2020 and July 2025 at two medical centers in the US. Data collected included medical history, blood pressure, and cholesterol levels.
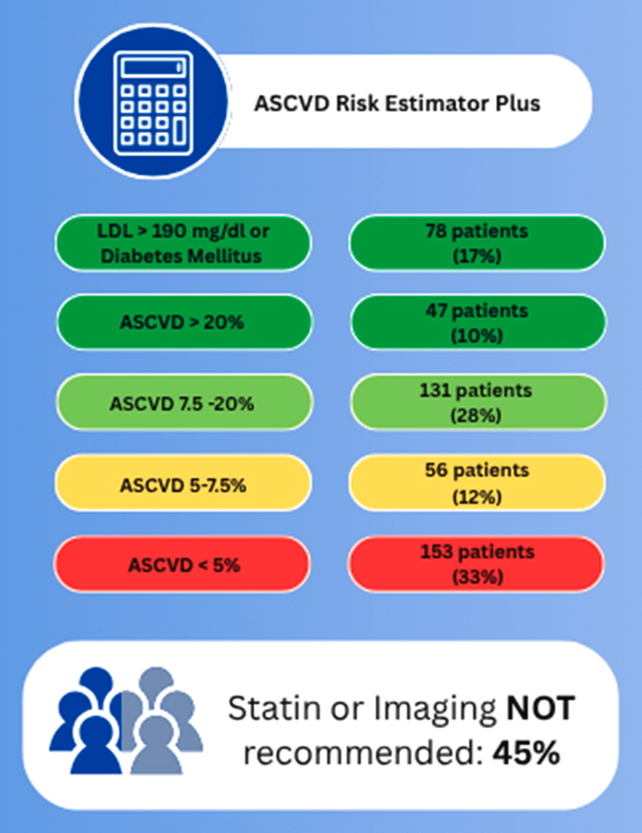
The analysis revealed that two days prior to their heart attack, 45 percent of the patients would have been classified as low or borderline risk levels using the ASCVD scores. An alternative scoring system known as predicting risk of cardiovascular disease events (PREVENT) performed even worse, categorizing 61 percent of patients as low or borderline risk.
Dr. Amir Ahmadi, a cardiologist at the Icahn School of Medicine at Mount Sinai in the US, emphasized the limitations of population-based risk tools in accurately assessing individual patients’ risk levels. He noted that nearly half of the patients would not have been recommended for further testing or preventive therapy based on current risk estimate scores and guidelines.
The current ASCVD score in the US is calculated during annual check-ups for individuals aged 40 to 75, predicting the risk of a heart attack or stroke within the next decade based on factors such as blood pressure, cholesterol levels, age, sex, and race.
Patients identified as being at intermediate or high risk of a heart attack, with high risk defined as a 20 percent or higher probability of an incident over the next ten years, are usually prescribed preventive measures like statins.
The researchers advocate for more comprehensive assessments of heart attack risk in asymptomatic groups – individuals not flagged by existing tools – potentially involving testing for atherosclerosis, the fatty plaques that obstruct blood flow in arteries.
Dr. Anna Mueller, an internal medicine resident at the Icahn School of Medicine at Mount Sinai, highlighted that most heart attacks occur in patients classified as low or intermediate risk, underscoring the importance of individualized risk evaluation beyond traditional symptoms.
While the study’s retrospective analysis focused on a limited number of cases, previous studies have demonstrated the efficacy of PREVENT scores in identifying heart attack risk in larger populations. Nonetheless, these scores still appear to overlook individuals without typical symptoms or risk factors.
By developing more personalized and effective approaches to heart disease assessment, early detection and prevention could be significantly enhanced, potentially reducing the incidence of heart attacks. Dr. Ahmadi stressed the need to move beyond current risk scores and symptoms as the primary determinants of preventive measures.
The findings of this study have been published in the Journal of the American College of Cardiology: Advances.




