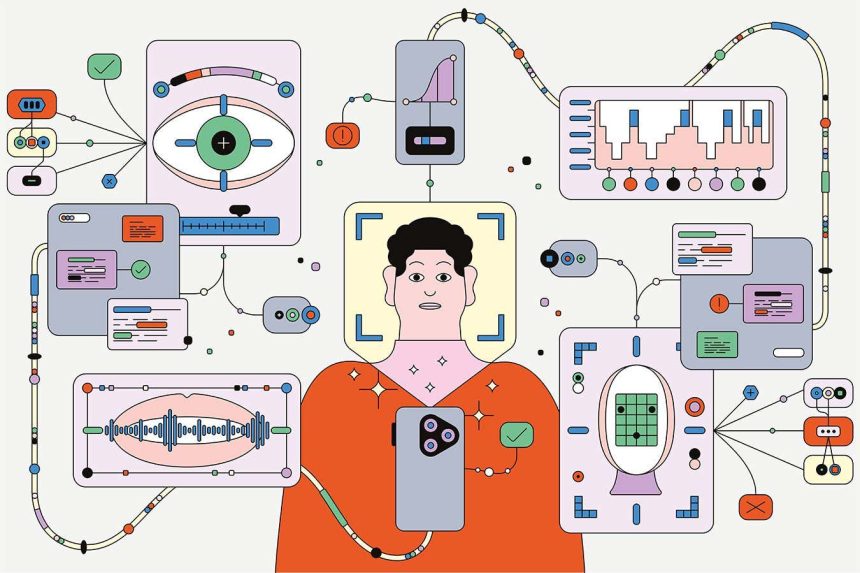
Researchers now hope that the advent of digital biomarkers could finally provide the breakthrough that has long eluded the field. These markers could offer a window into the subtle changes in behavior, physiology, and cognition that precede the onset of a mental health crisis. By analyzing data from smartphones, smartwatches, and other wearable devices, AI could potentially detect patterns that are invisible to the human eye.
For example, changes in the cadence of speech or the frequency of social interactions could indicate the early stages of depression or anxiety. Variations in heart rate or sleep patterns could signal the onset of a manic episode in bipolar disorder. By collecting and analyzing this data over time, AI could create personalized profiles for individuals and provide early warnings of potential relapses.
However, the use of AI in mental health diagnosis also raises important ethical and privacy concerns. How will this data be stored and protected? Who will have access to it, and how will it be used? Will individuals be able to opt out of having their data collected and analyzed? These are just a few of the questions that researchers and policymakers will need to address as this technology continues to evolve.
Despite these challenges, the potential benefits of digital biomarkers in psychiatry are clear. By providing a more objective and data-driven approach to diagnosis, AI could help improve treatment outcomes, reduce hospitalizations, and ultimately save lives. As technology continues to advance, it will be crucial for researchers, clinicians, and policymakers to work together to ensure that these innovations are used ethically and responsibly for the benefit of all.
There has been considerable excitement over the idea that certain people with depression exhibit high levels of bodily inflammation, leading to the suggestion that anti-inflammatory drugs could be used in treatment. However, despite this promising development, there are currently no accepted biomarkers for any mental health conditions.
Researchers have not been deterred by this slow progress and are now exploring the use of digital footprints to assess mental health. The concept began to gain traction in the mid-2010s as our reliance on smartphones and wearable devices increased, and recent advancements in artificial intelligence have further fueled interest in this area. The ability to analyze large datasets with AI has rapidly progressed in recent years.
Studies have identified potential biomarkers for depression, generalised anxiety disorder, social anxiety disorder, suicidality, and post-traumatic stress disorder. These conditions affect millions of people worldwide, and if digital biomarkers can be effectively implemented, they could significantly improve treatment monitoring.
Depression, in particular, has been a focus of research due to its high prevalence, affecting approximately 1 in 6 individuals over their lifetime. Early studies dating back to 2009 found that individuals with depression often exhibit flatter voices with reduced pitch variation. Similarly, facial expressions can also be indicative of an individual’s mental state. Subsequent research has suggested that vocal pitch changes could be used to identify different stages of bipolar disorder.
Deliberate AI, founded by Jeffrey Cohn, has expanded on these findings, incorporating various features such as speech patterns, head movements, muscle dynamics, and facial expressions to improve accuracy in diagnosing mental health conditions. The company is collaborating with researchers to study how biomarkers change during recovery, demonstrating high validity with existing measures.
One of Deliberate AI’s tools has been included in a pilot program with the US Food and Drug Administration, potentially qualifying its diagnoses as endpoints for clinical trials. The company is working to streamline the diagnostic process, utilizing short snippets of speech to achieve the same level of accuracy as full clinical interviews.
By combining AI chatbots with vocal and facial biomarker analysis, the hope is to improve accessibility to mental health diagnosis. Virtual encounters could help overcome barriers such as cost and availability of trained professionals, allowing individuals to track their symptoms regularly and accurately.
These advancements have practical implications, enabling psychiatrists to monitor treatment progress and adjust medication as needed based on changes in symptoms. Deliberate AI is also exploring the prediction of suicidal thoughts and behavior using biomarkers, with the goal of providing timely support to individuals at risk.
However, if you actually try to validate it scientifically, you might find that it doesn’t work at all,” he says. “It’s an area where there’s a lot of hype, but I think we need to be careful and critical about what we’re doing.”
Indeed, the field of digital biomarkers for mental health is still in its infancy, with many challenges and unknowns ahead. While AI and technology have the potential to revolutionize the way we diagnose and treat mental health conditions, they are not without their limitations. As researchers continue to explore and validate different biomarkers, it is important to remember that human connection and understanding are irreplaceable aspects of mental healthcare.
Ultimately, the goal should be to use technology as a tool to enhance, rather than replace, the human touch in psychiatry. By integrating digital biomarkers with traditional diagnostic methods and providing comprehensive support for individuals in need, we can create a more holistic and effective approach to mental health care.
As we move forward in this exciting and rapidly evolving field, it will be crucial to maintain a balance between innovation and caution, ensuring that the well-being and privacy of individuals remain at the forefront of our efforts. With thoughtful consideration and collaboration between researchers, clinicians, and individuals with lived experience, we can harness the power of AI and technology to improve mental health outcomes for all. Digital Biomarkers: Separating Hype from Hope
In a recent interview, researcher Mulinari expressed skepticism about the current hype surrounding digital biomarkers. He pointed out that labeling these markers as correlates of illness instead of actual causes can hinder funding opportunities. Despite this, Mulinari remains hopeful, drawing parallels to the initial excitement surrounding genetic sequencing in the early 2000s.
The comparison to genetic sequencing is apt, as the technology initially promised to revolutionize medicine but fell short of some lofty expectations. However, it has since become an integral part of modern healthcare. Mulinari believes that digital biomarkers have the potential to follow a similar trajectory, with initial hype eventually leading to significant breakthroughs.
Abi-Dargham shares Mulinari’s optimism, acknowledging the challenges but emphasizing the promise of digital biomarkers. She believes that these markers hold great potential for advancing our understanding of various health conditions.
While the field of digital biomarkers may be in its early stages, it is clear that researchers and healthcare professionals see the value in exploring this innovative approach. As with any new technology, there will be hurdles to overcome and expectations to manage. However, the potential benefits for personalized medicine and improved healthcare outcomes make the journey worthwhile.
For those seeking support during challenging times, resources like the UK Samaritans and US Suicide & Crisis Lifeline are available for assistance. It is important to prioritize mental health and reach out for help when needed.
In conclusion, the excitement surrounding digital biomarkers may be tempered by realistic expectations, but the potential for groundbreaking discoveries in healthcare is undeniable. As researchers continue to explore this emerging field, the hope is that digital biomarkers will lead to improved diagnostics, treatments, and ultimately, better health outcomes for all.