A Breakthrough in Life-Saving Surgery: Patient Kept Alive for 48 Hours Without Lungs
In a groundbreaking medical procedure, a team of surgeons managed to sustain the life of a critically ill man for 48 hours without his lungs while he awaited a double lung transplant. This innovative approach could potentially be a game-changer for selected patients in need of life-saving interventions.
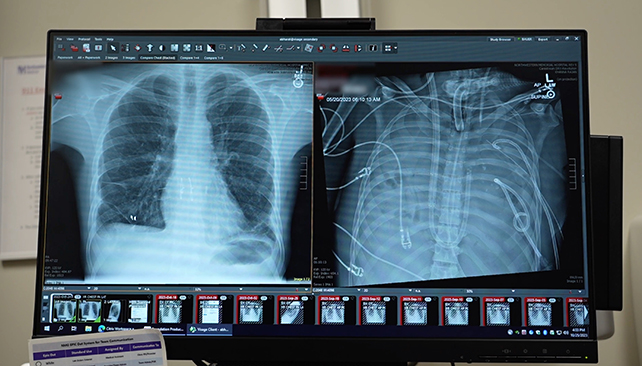
The team from Northwestern University in the US devised a Total Artificial Lung (TAL) system that mimics the oxygenation function of natural lungs, regulates blood flow, and safeguards the heart during this critical period. This artificial lung played a pivotal role in stabilizing the patient and preparing him for the eventual double lung transplant. Today, more than two years later, the patient has fully recovered and possesses fully functioning lungs.
Back in the spring of 2023, the 33-year-old man suffered from influenza-induced lung failure, which rapidly escalated to pneumonia, sepsis, and acute respiratory distress syndrome (ARDS). Thoracic surgeon Ankit Bharat explained that the infection in his lungs was untreatable with antibiotics, leading to liquefaction and systemic spread throughout his body.
Typically, a patient with severe lung issues would be placed on life support to allow the lungs to recover. However, in this unique case, the lungs were the primary source of infection, making their removal imperative for the patient’s survival. The decision to perform a bilateral pneumonectomy (removal of both lungs) posed a significant risk of heart failure due to disruptions in blood flow.
To address this challenge and surpass previous limitations, the medical team incorporated dual blood flow channels and a flow-adaptive shunt into the TAL system, ensuring stable blood circulation and preventing cardiac complications. The artificial lung sustained the patient long enough for his body to recuperate, making the lung transplant feasible. Post-surgery, signs of recovery from the infection became evident.
Through a molecular analysis of the extracted lungs, it was confirmed that spontaneous recovery from ARDS was unattainable due to extensive scarring and immune damage, necessitating a lung transplant. Bharat emphasized that while lung transplants are traditionally reserved for chronic conditions like interstitial lung disease, they can also be life-saving in acute cases of severe lung damage.
Published in Med, a case report detailing this extraordinary operation sheds light on the potential of such innovative approaches to save lives in critical situations. Bharat envisions the integration of these advancements into standard medical devices, making life-saving interventions more accessible to those in need.
Ultimately, this successful double lung transplant following temporary artificial lung support showcases the possibilities of modern medicine in overcoming seemingly insurmountable challenges. With timely access to donor organs, such procedures could offer hope to numerous patients facing life-threatening respiratory conditions.





