The landscape of lung cancer treatment is shifting, with a growing number of cases being diagnosed in individuals who have never smoked. This trend is prompting a reevaluation of screening recommendations and treatment strategies for this unique population.
While the absolute number of lung cancer cases in non-smokers is still a topic of debate, there is evidence to suggest that the proportion of cases in this group is increasing. Researchers are keen to understand the factors driving this trend and to explore potential screening options for never-smokers who may be at risk.
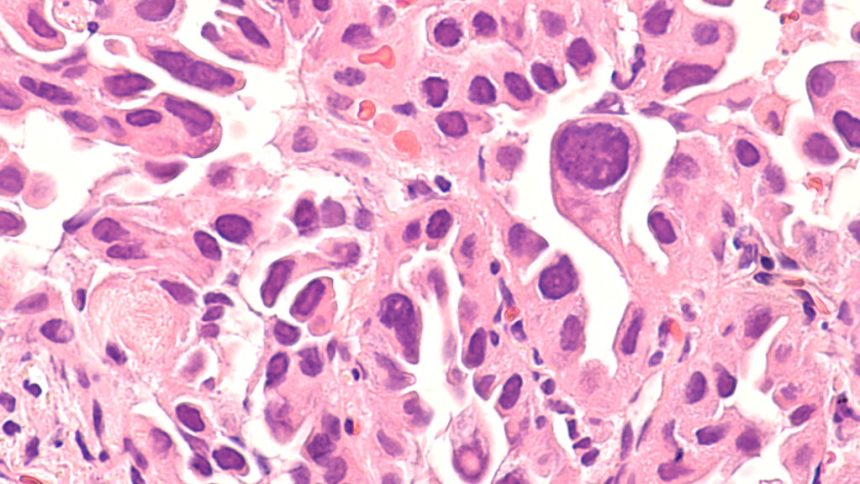
One key observation is that lung cancer in non-smokers often presents at more advanced stages, making it challenging to treat. These cases also exhibit specific genetic mutations that may respond well to targeted therapies, but the late diagnosis hampers the effectiveness of these treatments.
Women, in particular, seem to be at a higher risk of developing lung cancer despite never smoking. This could be attributed to hormonal or genetic factors, but environmental exposures such as air pollution and occupational hazards may also play a role. Screening efforts targeting never-smokers with a family history of the disease or those of Asian descent are being explored in various regions to identify high-risk individuals.
The symptoms of lung cancer in non-smokers can be nonspecific, leading to delays in diagnosis and treatment. Persistent coughs or unexplained pain are often overlooked, especially in younger individuals and women who do not fit the traditional profile of a lung cancer patient.
Recent studies in Taiwan and New York are investigating the outcomes of screening programs for never-smokers, aiming to identify individuals who could benefit from early detection and intervention. By understanding the unique characteristics of lung cancer in non-smokers and tailoring screening and treatment strategies accordingly, researchers hope to improve outcomes for this growing population of patients.
As the field continues to evolve, it is crucial to prioritize research funding and public health initiatives to address the changing epidemiology of lung cancer and ensure that all individuals at risk receive appropriate care and support. As we continue to learn more about cancer and its risk factors, it becomes increasingly important to identify those who may be at higher risk for developing the disease. Factors such as ethnicity, environmental exposure, and occupation can all play a role in determining an individual’s risk level.
For example, individuals of Asian descent may have genetic predispositions that make them more susceptible to certain types of cancer. Likewise, growing up in an area with high levels of air pollution can increase the risk of developing respiratory cancers. Additionally, certain occupations, such as working in a kitchen for long hours each day, can expose individuals to carcinogens that may increase their risk of developing cancer.
In light of these factors, it may be beneficial to consider implementing screening protocols for individuals who fall into these high-risk categories. For instance, individuals over the age of 60 who work in kitchens or have a history of exposure to air pollution may benefit from regular screenings to detect cancer at an early stage.
While there are ongoing trials and research efforts aimed at identifying high-risk individuals, more funding and resources are needed to further our understanding of cancer risk factors. By investing in research and screening programs, we can improve patient outcomes by detecting cancer earlier and providing timely interventions.
Ultimately, early detection is key in the fight against cancer. By identifying individuals at high risk and implementing targeted screening protocols, we can take proactive steps towards reducing the burden of cancer and improving overall patient outcomes.