alone and over 5.2 million deaths worldwide as of late 2024. But it was still a significant pandemic that caused a lot of illness, hospitalizations, and deaths.
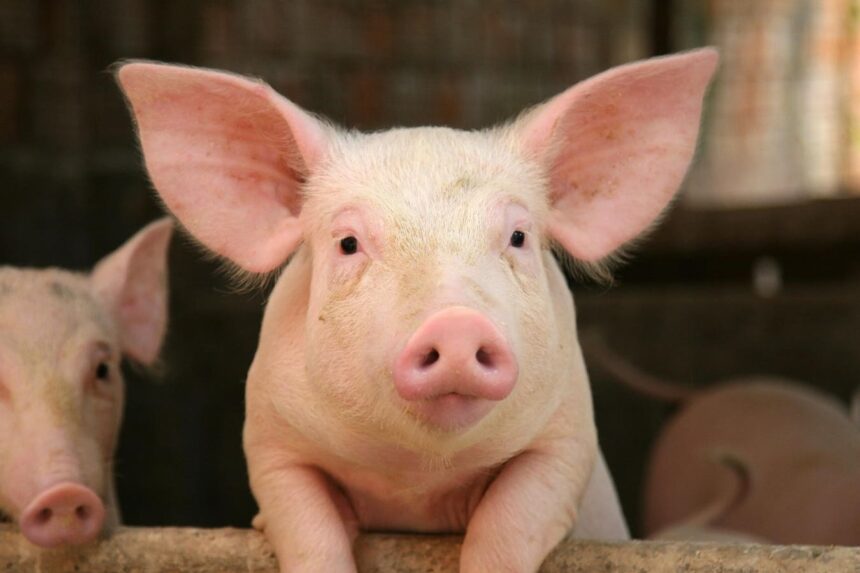
So, what if the H5N1 virus now spreading among birds, dairy cattle, and pigs reassorts again in pigs and creates a new virus that can jump to and spread among humans? That could potentially lead to another pandemic. While the H5N1 virus is currently not known to spread easily among humans, the potential for reassortment and the creation of a new virus with such capabilities is a real concern.
What Can Be Done to Prevent a Potential H5N1 Pandemic?
Preventing a potential H5N1 pandemic involves a multi-faceted approach. First and foremost, efforts to control and contain the spread of the virus among birds, cattle, and pigs are crucial. This includes strict biosecurity measures on farms, surveillance and testing of animals, and culling infected animals to prevent further spread.
Additionally, monitoring for any signs of genetic reassortment in pigs and other animals is important. Rapid identification of any new strains of the virus that may have the potential to spread to humans is essential for early intervention and prevention of a pandemic.
Finally, continued research into the H5N1 virus, its transmission and potential for reassortment, and development of vaccines and antiviral medications are also key components of pandemic preparedness.
While the public health risk of the H5N1 virus is currently considered low, vigilance and proactive measures are necessary to prevent a potential pandemic. Learning from past pandemics, such as the 2009 H1N1 pandemic, can help inform strategies to prevent and mitigate the impact of future outbreaks.
So, in conclusion, while the H5N1 virus may not be causing widespread panic at the moment, it is important to remain vigilant and proactive in monitoring and controlling its spread. The potential for genetic reassortment and the creation of a new virus with pandemic potential is a real concern that must be taken seriously. By learning from past pandemics and implementing effective prevention and control measures, we can hopefully avoid a repeat of history with the H5N1 bird flu.
The world has seen over 7 million deaths worldwide due to the ongoing pandemic, along with a growing number of long Covid cases. The impact of novel viruses on human populations can be unpredictable, as seen in past pandemics such as the 1918 flu outbreak that claimed an estimated 50 million lives. The H1N1 pandemic in 2009 was relatively milder due to some level of pre-existing immunity in older individuals.
Currently, there have been 55 confirmed cases of H5N1 bird flu in the U.S., with most cases linked to direct contact with infected animals. While human-to-human transmission has not been clearly documented, the potential for the virus to mutate and become more virulent remains a concern. Monitoring and surveillance of cases are crucial to track any changes in the virus’s behavior.
Despite the lessons learned from the COVID-19 pandemic, the U.S. appears to be repeating many of the same mistakes in preparing for another potential pandemic. Issues such as lack of comprehensive surveillance systems, healthcare system deficiencies, and personnel burnout continue to persist. The availability of effective antiviral medications and monoclonal antibodies against H5N1 is also limited.
Misinformation and disinformation pose a significant challenge in public health response efforts, with anti-science messages undermining preventive measures. Political leaders have not prioritized H5N1 preparedness, raising concerns about a lack of proactive measures to address future pandemics. It is crucial to focus on preparedness and preventive strategies to mitigate the impact of potential outbreaks.
In conclusion, while it is too early to predict the severity of the H5N1 bird flu threat, it is essential to prioritize preparedness and response efforts to ensure effective control of any emerging infectious diseases. Learning from past experiences and addressing current gaps in pandemic preparedness are critical to safeguarding public health in the face of evolving health threats. The world of technology is constantly evolving, with new innovations and advancements being made on a regular basis. One such advancement that has been gaining traction in recent years is the development of artificial intelligence (AI). AI is a branch of computer science that aims to create machines that can perform tasks that typically require human intelligence, such as speech recognition, decision-making, and visual perception.
One area where AI has been making significant strides is in the field of healthcare. AI has the potential to revolutionize the way we diagnose and treat medical conditions, by analyzing vast amounts of data and identifying patterns that may not be readily apparent to human doctors. This can lead to more accurate and timely diagnoses, as well as personalized treatment plans tailored to each individual patient.
For example, AI-powered diagnostic tools can analyze medical images such as X-rays and MRIs to detect abnormalities that may be missed by human radiologists. This can help to speed up the diagnosis process and ensure that patients receive the appropriate treatment as quickly as possible. AI can also be used to predict the likelihood of developing certain medical conditions based on a person’s genetic makeup, lifestyle factors, and medical history, allowing for early intervention and preventative measures to be implemented.
In addition to diagnosis and treatment, AI is also being used to improve patient care and streamline healthcare operations. Virtual health assistants powered by AI can provide patients with personalized advice and guidance on managing their health conditions, as well as reminders for medication and appointments. AI can also be used to optimize hospital workflows, such as scheduling surgeries and allocating resources more efficiently, leading to cost savings and improved patient outcomes.
While the potential benefits of AI in healthcare are vast, there are also challenges that need to be addressed. One major concern is the ethical implications of using AI in healthcare, such as ensuring patient privacy and data security, as well as preventing biases in AI algorithms that could impact patient care. There is also the issue of regulation and oversight, as the rapid pace of AI development means that laws and policies may struggle to keep up with the technology.
Overall, AI has the potential to revolutionize the healthcare industry and improve patient outcomes in ways that were previously unimaginable. By harnessing the power of AI, we can unlock new possibilities for diagnosis, treatment, and patient care, ultimately leading to a healthier and more efficient healthcare system for all.