Male fertility is a topic of increasing concern, with a new study suggesting that medical conditions like sleep apnea may be contributing to the decline in sperm quality and overall reproductive health in men. Published in Nature Reviews Urology, the study led by Dr. Tessa Lord from the University of Newcastle explores the impact of factors such as sleep apnea, varicocele, and high-altitude exposure on male fertility.
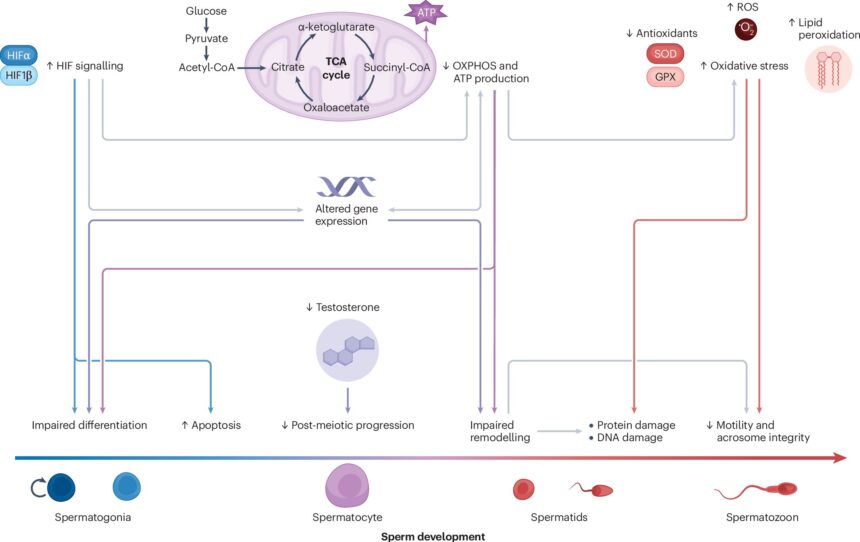
One of the key findings of the review is the role of testis hypoxia in impairing spermatogenesis and sperm function. Testis hypoxia, a condition where the testes are deprived of oxygen, can negatively impact sperm count and quality by disrupting hormone production and gene expression. Conditions like varicocele and sleep apnea are known to reduce the level of oxygenated blood in the testis, leading to sustained threats to reproductive health.
Varicocele, a common abnormality characterized by enlarged veins in the scrotum, is a known cause of infertility in up to 45% of men struggling to conceive. Similarly, obstructive sleep apnea, a prevalent sleep disorder affecting 13%-30% of men, has been linked to infertility in males. Further research is needed to understand the direct effects of sleep apnea on sperm production and quality.
Interestingly, high-altitude activities like hiking can also cause testis hypoxia, but the effects on fertility are usually temporary and reversible once oxygen levels are restored. Dr. Lord emphasizes the importance of timely management of conditions like varicocele and sleep apnea to mitigate fertility risks associated with testicular hypoxia.
The review also highlights the urgent need to uncover potential intergenerational effects of testicular hypoxia on male fertility trends. Dr. Lord points out that emerging evidence suggests that fathers experiencing testis hypoxia could pass on developmental issues to their offspring, leading to fertility issues in future generations. More research is needed to fully understand the generational impact of testicular hypoxia and develop effective interventions to improve fertility outcomes.
In conclusion, the study underscores the critical role of testis hypoxia in male fertility and calls for greater awareness of the reproductive risks associated with sustained lack of oxygen in the testes. By addressing underlying medical conditions that cause testicular hypoxia, we can potentially reverse subfertility and safeguard the reproductive health of current and future generations.