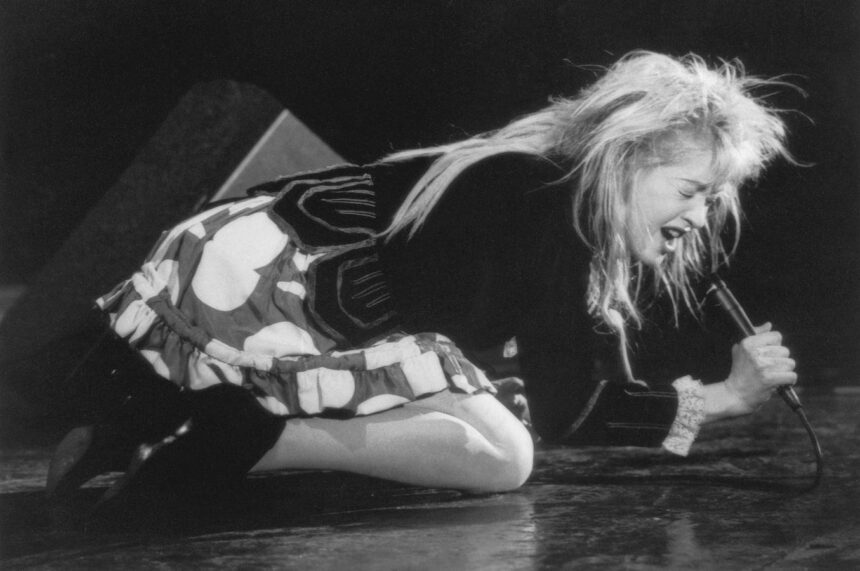
Financial incentives have always been a powerful motivator, whether in the realm of love or professional practice. Cyndi Lauper’s iconic song “Money changes everything” captures this sentiment perfectly. Recent studies have shed light on how money can influence surgical practices, offering valuable insights into the dynamics of financial incentives for healthcare professionals.
One study, published in JAMA, focused on the impact of a new Medicare billing code for abdominal hernia repair. This code rewarded surgeons with higher payments for hernias measuring at least 3 centimeters in size. The results were intriguing, with a noticeable shift in the percentage of patients categorized as having smaller, lower-payment hernias. This change raised questions about the accuracy of hernia size measurements and the potential influence of financial incentives on clinical decision-making.
The researchers highlighted the phenomenon of “perceptive bias” and the risk of dishonest behavior when financial incentives are introduced into medical practice. The study underscored the complexity of aligning financial incentives with quality patient care, emphasizing the need for transparency and accountability in billing practices.
In another study, researchers examined the use of financial incentives to promote active surveillance for low-risk prostate cancer patients. Despite the potential for improvement in patient outcomes and cost savings, the results were disappointing. The payment incentive did not lead to increased utilization of active surveillance among patients with low-risk disease.
The findings raised important questions about the factors driving treatment decisions in healthcare settings. Nonclinical considerations, such as financial incentives and reimbursement policies, were identified as potential influencers of surgical practices. The researchers emphasized the need for reimbursement parity between different management strategies to ensure that financial incentives align with quality patient care.
Overall, the studies highlighted the complex interplay between financial incentives and clinical decision-making in surgical practice. While money can be a powerful motivator, its impact on healthcare delivery must be carefully considered to ensure that patient outcomes are prioritized. By reevaluating reimbursement policies and promoting transparency in billing practices, healthcare systems can strive towards a more patient-centered and value-based approach to surgical care. The world of technology is constantly evolving, with new innovations and advancements being made every day. One of the most exciting areas of technology that is currently seeing rapid growth is artificial intelligence (AI). AI is a branch of computer science that aims to create intelligent machines that can think, learn, and solve problems like humans.
One of the key applications of AI is in the field of healthcare. AI has the potential to revolutionize the way we diagnose and treat diseases, making healthcare more efficient and effective. For example, AI-powered algorithms can analyze medical images, such as X-rays and MRIs, to detect abnormalities and diagnose conditions with a high level of accuracy. This can help doctors make more informed decisions and provide better care to patients.
AI is also being used to develop personalized treatment plans for patients. By analyzing large amounts of data, AI can identify patterns and trends that can help doctors tailor treatment plans to individual patients based on their unique characteristics and medical history. This can lead to better outcomes and reduce the risk of adverse effects from treatments.
Another exciting application of AI in healthcare is in drug discovery. Developing new drugs is a long and expensive process, but AI has the potential to speed up this process by analyzing vast amounts of data to identify potential drug candidates. This can help researchers identify new treatments for diseases more quickly and efficiently.
AI is also being used to improve the efficiency of healthcare systems by optimizing processes and reducing costs. For example, AI-powered chatbots can help patients schedule appointments, answer questions, and provide basic medical advice, freeing up healthcare professionals to focus on more complex tasks. AI can also help hospitals and healthcare facilities streamline operations, reduce administrative burden, and improve patient outcomes.
Despite the many benefits of AI in healthcare, there are also challenges and concerns that need to be addressed. One of the main concerns is the ethical implications of using AI in healthcare, such as ensuring patient privacy and data security. There are also concerns about the potential for bias in AI algorithms, which could lead to disparities in healthcare outcomes for certain groups of patients.
Overall, AI has the potential to revolutionize the healthcare industry and improve patient care in ways we never thought possible. By harnessing the power of AI, we can make healthcare more efficient, effective, and personalized, ultimately leading to better outcomes for patients around the world.