The House Republican budget reconciliation legislation, known as “the big, beautiful bill,” has stirred controversy due to its potential impact on healthcare coverage for millions of Americans. According to the Congressional Budget Office, nearly 11 million people could lose their health insurance over the next nine years if the bill is enacted. Specifically, around 7.8 million individuals may lose Medicaid coverage if strict work requirements and eligibility checks are enforced, while several million more could lose coverage through changes to the Affordable Care Act exchanges.
The proposed budget includes significant cuts of $715 billion in Medicaid and $300 billion in the Supplemental Nutrition Assistance Program. It seeks to implement work requirements for able-bodied childless adults, impose co-payments for those above 100% of the federal poverty level, and tighten eligibility verification. Additionally, penalties may be imposed on states that provide healthcare coverage to certain immigrants.
The work requirements, which apply to both Medicaid and SNAP, are set to begin in 2026. Despite a majority of Medicaid beneficiaries already being employed, in school, or caregivers, the bill is projected to reduce Medicaid enrollment by nearly eight million individuals. Changes to the ACA marketplace could also result in higher out-of-pocket costs for coverage plans and make it harder for individuals to enroll due to shorter enrollment windows and increased paperwork.
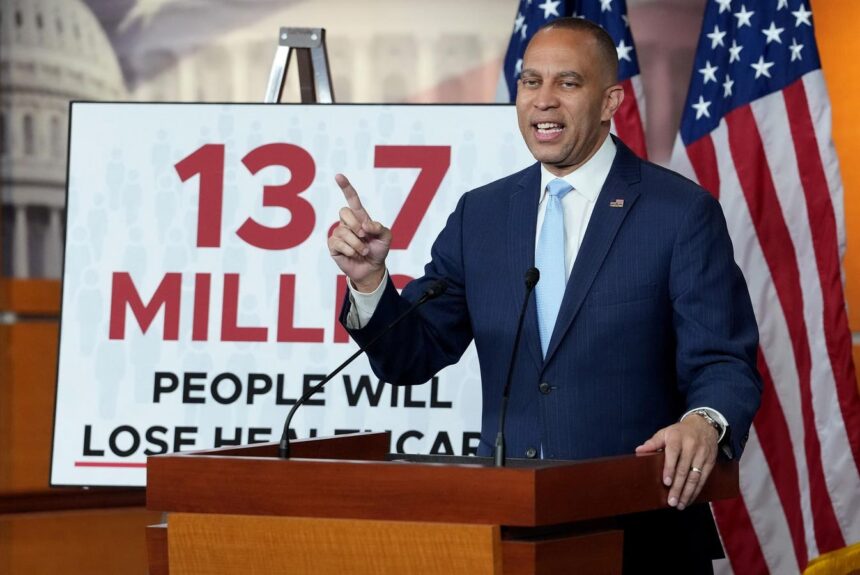
Critics of the bill, including House Minority Leader Hakeem Jeffries, argue that the number of uninsured individuals could reach up to 13.7 million due to the elimination of ACA premium subsidies. On the other hand, Republicans like Senator James Lankford claim that those losing Medicaid coverage could transition to employer-based healthcare. However, not all employers offer health insurance, raising concerns about access to coverage for those affected by the bill.
Moreover, the reconciliation package includes over $500 billion in automatic cuts to Medicare spending, potentially impacting Medicare eligibility for certain migrant groups and leading to reductions in payments to healthcare providers. The legislation also aims to regulate pharmacy benefit managers (PBMs) in Medicare drug plans by limiting their compensation and establishing transparency requirements.
While the bill’s provisions aim to address healthcare costs and program efficiency, there are concerns about the potential consequences for access to care and affordability for vulnerable populations. The Senate will likely review and potentially amend the bill before it becomes law, considering the widespread opposition and implications of the proposed changes.