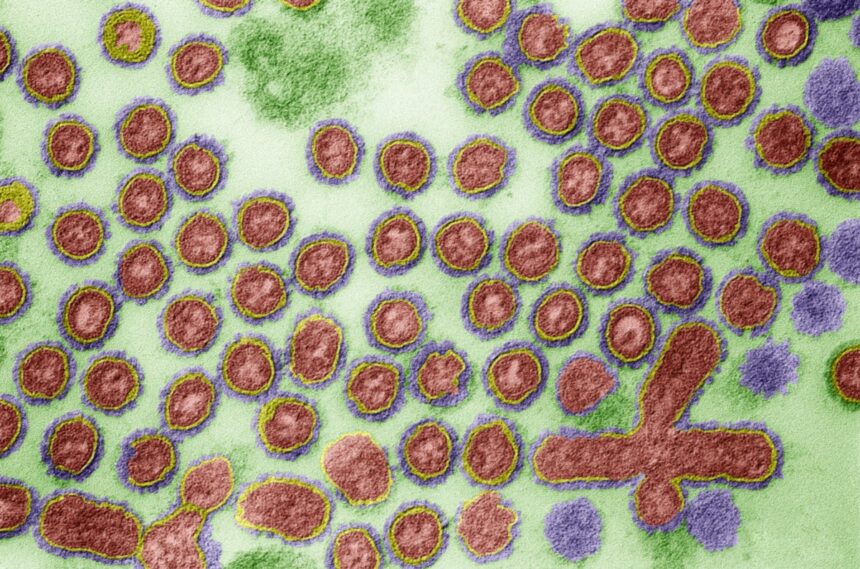
The emergence of H5N1 bird flu in the United States has raised concerns among health officials and scientists. This strain of avian influenza is showing unique characteristics, spreading to new species and locations in ways not previously observed. The virus has already infected 36 people in six U.S. states, including California, Colorado, Michigan, Missouri, Texas, and Washington. However, the actual number of cases may be higher due to limited testing and flawed diagnostic tools.
Despite the relatively low number of human infections so far, experts are closely monitoring the situation. While H5N1 typically causes mild symptoms in humans and does not easily transmit between people, there is always the risk of the virus mutating into a more dangerous form. The prospect of a pandemic flu outbreak is a cause for concern, especially given the rapid spread of diseases like COVID-19.
The U.S. government is taking steps to prepare for a potential H5N1 pandemic, including stockpiling vaccines. However, the current supply of vaccines is limited, with only enough doses to fully vaccinate a small fraction of the population. The lack of a licensed mRNA vaccine for flu is a significant challenge, as traditional egg-based vaccines are slower to produce and may not be effective against rapidly evolving strains.
Moderna and Pfizer, both known for their mRNA COVID-19 vaccines, are working on H5N1 flu vaccines, but these are still in development. The slow progress in vaccine development highlights the difficulties in preparing for novel flu strains that can quickly spread and cause severe illness. Scientists like Scott Hensley are working on innovative vaccine technologies that could be more adaptable to new flu strains, but progress has been hampered by competing priorities such as the COVID-19 pandemic.
In the face of uncertainty surrounding the H5N1 virus, it is crucial to remain vigilant and prepared for the possibility of a pandemic outbreak. Public health officials emphasize the importance of early detection, rapid response, and global cooperation to mitigate the impact of emerging infectious diseases. By learning from past experiences and investing in innovative research, we can better prepare for future health threats and protect the well-being of communities worldwide. In the midst of a constantly evolving flu virus, government agencies, flu vaccine makers, and researchers are facing a challenging task. They must closely monitor the virus, hoping to detect any changes and develop the right vaccine in a timely manner. As Dr. Johnson mentioned at a recent meeting, it’s impossible to maintain a large stockpile of vaccines due to the virus’s continuous evolution.
One potential solution to this dilemma is the development of a universal flu vaccine. This vaccine would offer protection against all strains of flu by helping the immune system recognize consistent parts of the virus across different seasons and strains. Dr. Khan advocates for a “moonshot project” to create a universal flu vaccine that could safeguard against both seasonal flu and new pandemic strains, such as the H1N1 strain that emerged in 2009.
While progress has been made in developing an mRNA vaccine that provides immunity against all known influenza subtypes, it is not a universal flu vaccine but rather a primer for initial protection. This type of vaccine could help address the issue of stockpiling vaccines, as ongoing production would be more efficient than one-time efforts.
Despite years of research, no lab has successfully produced a vaccine that protects against flu subtype mutations that cause seasonal drift. Additionally, there has been little political support for such endeavors, with public skepticism towards vaccines on the rise. The lack of trust in vaccines, as evidenced by declining childhood vaccination rates and low COVID vaccination numbers, poses a significant challenge to pandemic preparedness.
As some states relax vaccine requirements and recommendations, public health experts like Dr. Khan are concerned about the potential consequences. Without widespread vaccination, individuals remain vulnerable to future pandemics. It is crucial for politicians to prioritize pandemic preparedness and promote vaccine uptake to mitigate the impact of future outbreaks.
In conclusion, the development of a universal flu vaccine remains a critical goal in addressing the ever-changing nature of the flu virus. It is essential for policymakers, healthcare providers, and the public to work together to ensure that vaccines are widely accessible and trusted. By investing in research and public health initiatives, we can better prepare for the next pandemic and protect the health and well-being of our communities.