A Breakthrough in Cancer Therapy: CAR T-Cell Treatment Keeps Patient Free of Tumour for 18 Years

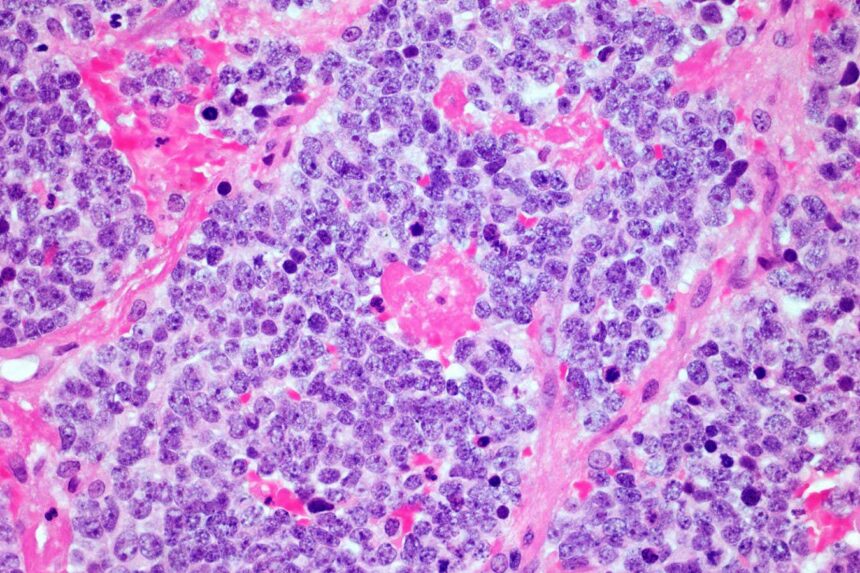
A microscopic image of a neuroblastoma tumour
Simon Belcher/Alamy
Groundbreaking research has revealed that a novel cancer therapy utilizing genetically engineered immune cells, known as CAR T-cells, has achieved a remarkable feat by keeping a patient free of a potentially fatal nerve tumour for an unprecedented 18 years.
According to Karin Straathof from University College London, this case represents the longest-lasting complete remission ever observed in a patient treated with CAR T-cell therapy, leading to the conclusion that the patient has been cured of their condition.
CAR T-cell therapy is commonly employed in the treatment of certain blood cancers, such as leukaemia. The process involves extracting T-cells from the patient’s bloodstream, genetically modifying them to target and eliminate cancer cells, and then reintroducing these modified cells back into the body. Recent studies have shown success in putting individuals with leukaemia into remission for extended periods, with a record remission of 11 years reported in 2022.
However, CAR T-cell therapy has historically struggled to combat solid tumours like neuroblastoma, a form of cancer that affects nerve cells in children. These tumours often exhibit strong resistance to immune system attacks, hampering the effectiveness of modified T-cells.
Despite these challenges, Cliona Rooney and her team at Baylor College of Medicine in Houston were astonished to discover that a patient treated with CAR T-cell therapy for neuroblastoma in 2005 remained cancer-free after more than 18 years. Rooney described these results as remarkable, given the rarity of complete responses in neuroblastoma cases using this approach.
The individual in question received the treatment at the age of 4 after conventional chemotherapy and radiotherapy failed to eradicate the cancer completely. Out of 10 other participants with neuroblastoma who underwent the same treatment, one individual showed no signs of cancer nearly nine years later before exiting the study. Tragically, the remaining participants succumbed to their cancer within a few years post-treatment.
It remains unclear why some patients responded more favorably to the therapy than others. Rooney suggests that variations in T-cell behavior influenced by genetic factors, prior infections, and lifestyle choices could play a role. Additionally, differences in tumour immunosuppression levels may affect the response to CAR T-cell therapy.
Rooney’s team is now focused on enhancing the potency of engineered cells to benefit a larger population of patients while minimizing potential side effects. These ongoing efforts are expected to lead to further advancements in cancer treatment, as Straathof believes that the current success story offers a glimpse into the future possibilities of this innovative therapy.
Topics: