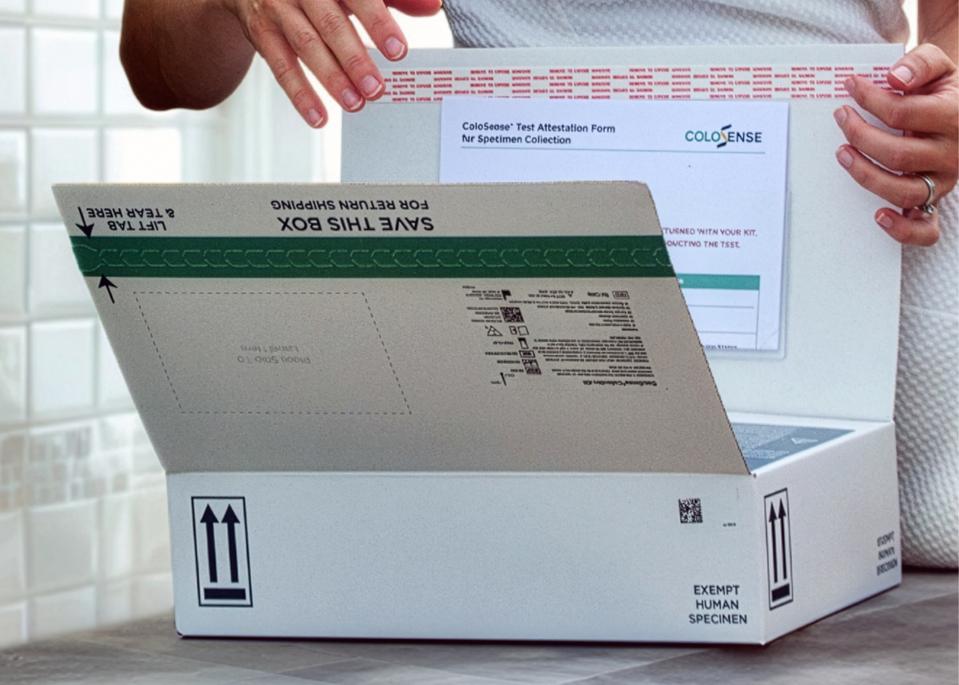
ColoSense box being opened by a patient
ColoSense
Actor James Van Der Beek, known for his role in Dawson’s Creek, recently shared his diagnosis of stage 3 colon cancer at the age of 47, after exhibiting warning signs of the disease. As a physician, I frequently encounter cases where symptoms of colon cancer—such as rectal bleeding, changes in bowel habits, unexplained weight loss, or abdominal discomfort—go unacknowledged as serious concerns. Even more alarming is the fact that numerous individuals remain unaware that the recommended age for screening was recently lowered from 50 to 45, adding 19 million people to the eligible screening pool. Van Der Beek’s candid sharing emphasizes the critical importance of recognizing symptoms and initiating early screenings.
Although colonoscopy continues to be the benchmark for prevention, its accessibility can be limited. Hence, innovative non-invasive screening methods, such as the recently FDA-approved ColoSense, are making headway in expanding access to colon cancer screening.
Colon Cancer: A Growing Healthcare Concern
Colon cancer, commonly referred to as colorectal cancer, affects the colon and rectum of the large intestine. Research shows that since the 1990s, the prevalence of colon cancer among individuals under 50 has been rising by 1-2% annually. In recent years, I have increasingly seen young adults in their 20s and 30s battling advanced stages of colon cancer. A common factor among many of these patients is a lack of awareness regarding symptoms, risk factors, and the recommended age for routine screening.
Education for both patients and healthcare providers is crucial in curbing the increase in colon cancer incidences. However, awareness must be accompanied by access, which is currently limited.
The Challenges of Colonoscopy Accessibility
Photo of Dr. Erica Barnell
ColoSense
Dr. Erica Barnell, co-founder and Chief Medical and Science Officer of Geneoscopy, remarks, “With the recent lowering of the screening age, millions more individuals are eligible. However, the number of gastroenterologists and available colonoscopy appointments is insufficient to meet the heightened demand.” Currently, approximately 44 million Americans qualify for screening, but there are only around 17,000 gastroenterologists actively practicing, and over half are nearing retirement age. Complicating matters is the fact that colon cancer rates are increasingly seen in those under 45, prompting some policymakers to suggest a further reduction in the screening age to 35, which could exacerbate the existing strain on the healthcare system.
To enhance screening accessibility and alleviate the load on colonoscopy procedures, Geneoscopy has introduced ColoSense, a non-invasive screening tool that utilizes stool samples to identify colon cancer and precancerous conditions. Approved by the FDA in May 2024, ColoSense is part of the latest advancements in non-invasive methods for average-risk patients. Rather than relying on methylation-based stool DNA tests, ColoSense employs RNA biomarkers to detect cancer and precancerous indicators.
In pivotal trials, the RNA-based stool test successfully identified 93% of colorectal cancer cases and 45% of advanced adenomas, while accurately ruling out lesions in 88% of individuals. Compared to traditional fecal immunochemical tests (FIT), it showcased significantly higher sensitivity for both cancers (93% versus 78%) and precancerous growths (45% versus 29%). Barnell adds that “ColoSense demonstrated strong sensitivity across all ages.”
Streamlining Colon Cancer Screening with ColoSense
ColoSense delivered to a patient’s front door
ColoSense
Designed for patient comfort and convenience, ColoSense simplifies the stool sample collection process. Unlike other tests that involve complex procedures, the ColoSense kit allows for easy stool collection, which can then be sent via FedEx to the lab for analysis, with results communicated to both patients and their healthcare providers.
Crucially, ColoSense is intended to complement, rather than replace, colonoscopy. Individuals with positive results will still require a colonoscopy for confirmation and potential polyp removal. However, by pinpointing those who are most likely to need further testing, non-invasive options can alleviate the burden on the healthcare system, ensuring that colonoscopy capacity is reserved for higher-risk patients.
Cost, Coverage, and Navigating Care with ColoSense
Despite its FDA endorsement, obstacles regarding non-invasive tests and insurance coverage persist. Fortunately, ColoSense is witnessing increasing acceptance from private insurance companies and state Medicaid plans, while it is also undergoing review for Medicare coverage. Priced at $508.87, as established by the Centers for Medicare & Medicaid Services, patients can opt to pay out-of-pocket if necessary. Nevertheless, Barnell stresses, “Our goal is for no patient to bear out-of-pocket costs when their provider orders the test.”
To further combat inequities, ColoSense offers comprehensive care navigation, assisting patients in connecting with local healthcare providers after receiving positive results, thus facilitating timely colonoscopy appointments for further evaluation and possible treatment. This strategy seeks to alleviate both financial and logistical barriers that may hinder many from completing their screening.
Colonoscopy: The Proven Gold Standard
While the ease, affordability, and accessibility of ColoSense enhance screening and early detection capabilities, the colonoscopy remains the gold standard. Patients often express concern regarding the preparation process—temporary dietary changes and bowel cleansing—which is widely acknowledged as the most daunting aspect. The procedure itself typically lasts about 30 minutes and is conducted under sedation, offering same-day recovery.
Serious complications, such as perforation or bleeding, are exceedingly rare, and the advantages—such as the removal of polyps before they develop into cancer—are life-saving. Proper assessments are essential to ensure the patient is safe during preparation and the procedure.
Colonoscopy is particularly recommended for high-risk individuals, including those with a family history of colorectal cancer, genetic predispositions, or previous concerning findings on imaging. For average-risk patients unable to undergo colonoscopy, ColoSense presents a valuable FDA-approved, noninvasive alternative.
The Ongoing Need for Patient Education and Advocacy
The importance of education for both patients and healthcare providers cannot be overstated.
James Van Der Beek’s experience exemplifies the potential consequences that may occur when subtle symptoms align with a lack of awareness regarding colon cancer. His willingness to share his journey plays a vital role in educating others, ultimately contributing to life-saving outcomes. The medical community—and patients alike—greatly appreciates his advocacy.





