New Study Shows Link Between Psychiatric Medications and ALS Risk
A recent study conducted by researchers at the Karolinska Institute in Sweden has revealed a potential connection between certain psychiatric medications and an increased risk of developing amyotrophic lateral sclerosis (ALS), the most common form of motor neurone disease (MND).
The study focused on medications such as anxiolytics, hypnotics and sedatives, and antidepressants – commonly prescribed for conditions like anxiety, depression, and sleep disorders. The research found that individuals taking these medications had a 34 percent, 21 percent, and 26 percent higher risk of developing ALS, respectively.
While the overall risk increase is relatively small in comparison to the low prevalence of ALS, understanding these associations could provide valuable insights for the treatment of both psychiatric disorders and motor neurone diseases.
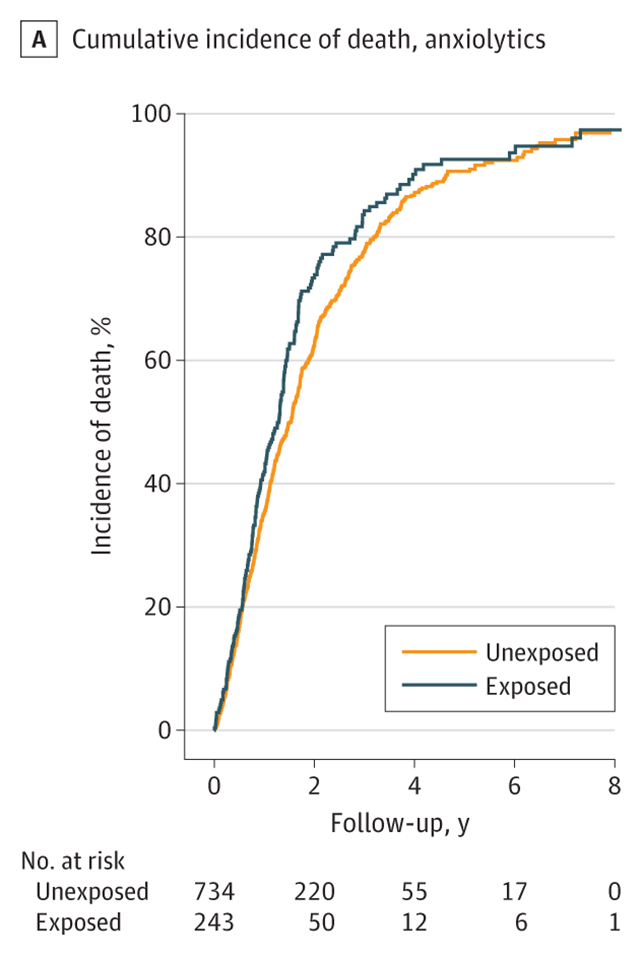
In their published paper, the researchers noted, “Prescribed use of anxiolytics, hypnotics and sedatives, or antidepressants was associated with a higher subsequent risk of ALS. Prediagnostic use of such medications was also associated with a poor prognosis after ALS diagnosis.”
ALS, a progressive neurodegenerative disease that leads to paralysis and respiratory failure, currently has no cure. The study also highlighted a slightly faster rate of decline and an increased risk of premature death among ALS patients who had been exposed to psychiatric medications.
The researchers utilized national health data from Sweden to compare ALS patients with a control group, accounting for genetic and environmental factors in their analysis. While the study does not definitively prove causation, it suggests a potential link between psychiatric medications and ALS risk.
Neuroscientist Susannah Tye from the University of Queensland commented on the study, stating, “This study adds to growing evidence that individuals with psychiatric conditions may face an elevated risk of neurodegenerative diseases such as ALS. However, the implication that psychiatric medications themselves contribute to this risk should be interpreted with caution.”
Despite the rarity of ALS, affecting approximately 9 in 100,000 people in the US, the study sheds light on the complex interplay between psychiatric disorders, medication use, and neurodegenerative diseases. While millions of individuals take psychiatric medications without developing ALS, understanding these connections could lead to advancements in treatment strategies for both conditions.
As research continues to uncover the factors influencing ALS risk, there is hope for improved treatments and potential breakthroughs in addressing this debilitating disease. The study has been published in JAMA Network Open.





