Bacteria in stools could be an unexpected weapon in the fight against cancer
When traditional cancer treatments fail to produce the desired results, a novel approach involving faecal transplants from individuals who have successfully responded to a specific type of cancer treatment may offer a promising alternative. Recent research indicates that altering the gut microbiome through faecal microbiota transplantation (FMT) can have a significant impact on the immune system, leading to the stabilization of tumours in individuals with kidney cancer.
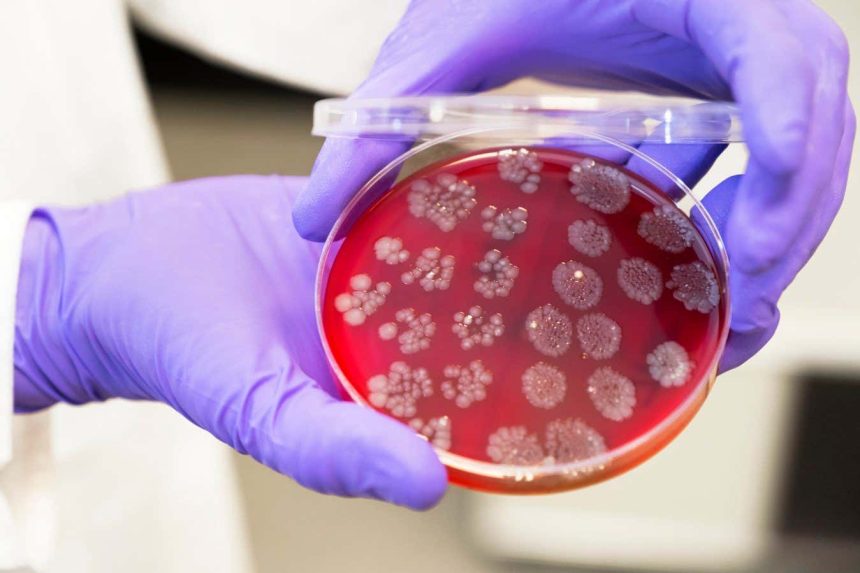
FMT is a procedure that entails transferring stool samples from a healthy donor to the gut of a recipient with the aim of improving their microbiome composition. While FMT is currently approved for treating recurrent antibiotic-resistant Clostridioides difficile infections, it has also shown potential in addressing other conditions such as irritable bowel syndrome.
Immunotherapy drugs known as checkpoint inhibitors have demonstrated efficacy in helping the immune system target and destroy cancer cells. However, these drugs do not work for everyone. Previous studies have suggested that administering FMT from individuals who respond positively to checkpoint inhibitors to non-responders could enhance treatment outcomes. By modulating the microbiome, researchers believe they can boost immunity and enhance the body’s ability to combat cancer.
In a recent study conducted by Gianluca Ianiro and his team at the Catholic University of the Sacred Heart in Rome, Italy, 45 adults with kidney cancer were enrolled in a trial. Participants who had recently initiated treatment with pembrolizumab, a checkpoint inhibitor, and axitinib, a drug that targets tumour blood supply, were randomly assigned to receive either a faecal transplant from a cancer remission patient or a saline solution.
Results from the study revealed that individuals who received the faecal transplant exhibited stable cancer progression for an average of two years following the procedure, compared to only nine months in the placebo group. Additionally, over half of the participants in the FMT group experienced tumour shrinkage, a significant improvement compared to the placebo group.
According to Hassane Zarour from the University of Pittsburgh, the study’s findings strengthen the evidence supporting the therapeutic manipulation of the gut microbiome to influence immunotherapy outcomes. The introduction of a specific gut bacteria species called Blautia wexlerae through the faecal transplant was linked to the production of short-chain fatty acids known to promote anti-cancer immune cells.
Moreover, faecal transplants were found to alter the levels of existing gut bacteria in recipients, reducing harmful inflammation-promoting strains and increasing beneficial bacteria that support the production of short-chain fatty acids. These findings align with another study demonstrating the efficacy of FMT in enhancing the effects of checkpoint inhibitors in individuals with non-small cell lung cancer.
Ongoing research is exploring the potential of FMTs in treating other tumour types that respond to checkpoint inhibitors, such as bladder and head and neck cancers. Large-scale randomized controlled trials are necessary to validate these findings and identify the specific bacterial strains within faeces that offer therapeutic benefits. This knowledge could pave the way for the development of artificial microbial samples tailored for cancer treatment on a broader scale.