The rapid development of secondary lung infections following upper respiratory tract infections has always been a major concern, especially for vulnerable populations such as children and the elderly. These secondary infections, like pneumonia, can escalate quickly and pose a serious threat to health. However, the mechanisms behind the swift progression from upper respiratory symptoms to deep lung infections have long puzzled scientists and medical professionals.
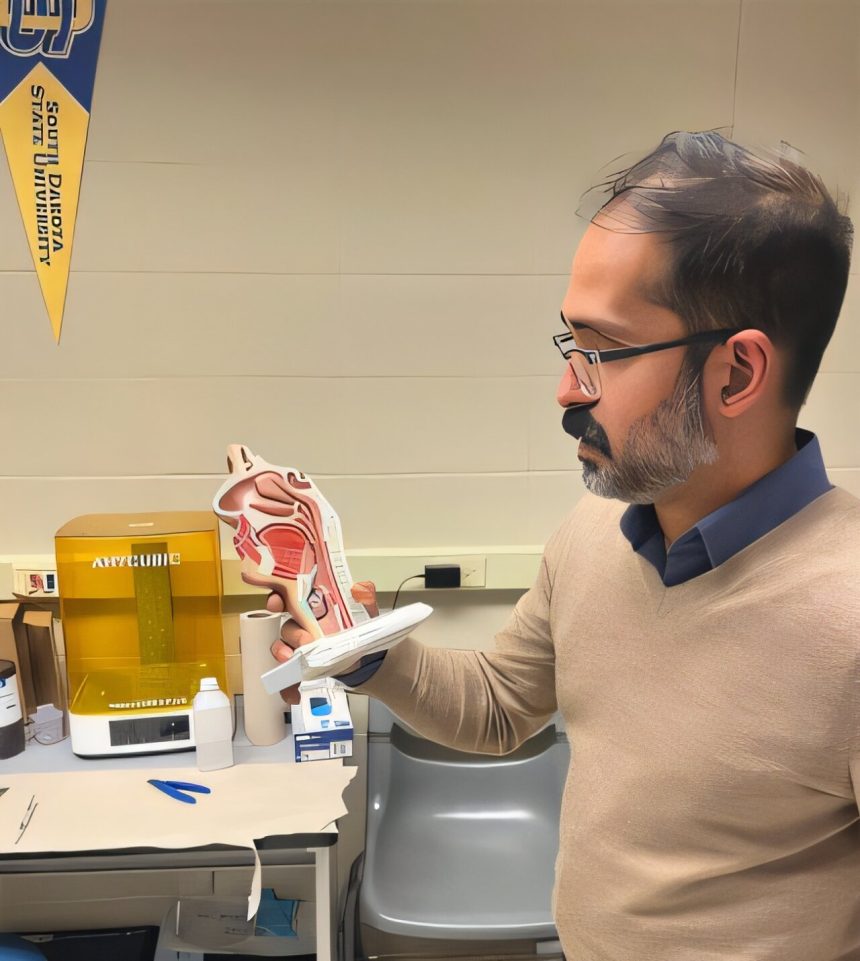
A recent study conducted by Saikat Basu, an associate professor at South Dakota State University’s Department of Mechanical Engineering, sheds light on this issue. Published in the journal PLOS One, Basu’s research delves into the intricate dynamics of infection transmission in the human airways, particularly focusing on the lower airway mechanics.
Basu, who specializes in fluid mechanics and biomathematical modeling, has been at the forefront of interdisciplinary research, especially during the COVID-19 pandemic. His previous work on respiratory transport and viral infections has been groundbreaking and has paved the way for his latest study on secondary lung infections.
Through computational simulations of respiratory fluid physics within 3D models of human airways, Basu discovered that mucus fragments from initial infection sites in the upper airway can easily be inhaled into the lungs. These microdroplets, some as large as 15 to 20 micrometers, carry high viral loads and act as efficient carriers of pathogens to the bronchial spaces.
The relatively straight structural shape of the laryngotracheal cavity facilitates the downward motion of these mucus fragments, allowing them to reach the lungs quickly. Basu’s research explains how these particles, above the infectious threshold, can lead to the rapid onset of secondary lung infections after initial upper respiratory tract infections.
By providing a plausible explanation for the swift progression of illnesses from the throat to the lungs, Basu’s findings offer valuable insights for predicting and preventing secondary infections. This research not only deepens our understanding of infection transmission in the human airways but also sets the stage for further exploration in bronchial biophysics.
Overall, Basu’s study highlights the critical role of fluid mechanics in understanding the development of secondary lung infections and underscores the importance of interdisciplinary research in addressing complex health challenges. This research has the potential to revolutionize our approach to respiratory infections and enhance our ability to protect vulnerable populations from serious complications.