This case highlights the urgent need for global cooperation in combating antimicrobial resistance. The misuse and overuse of antibiotics have led to the emergence of multidrug-resistant bacteria, posing a serious threat to public health worldwide. As more and more bacteria develop resistance to existing treatments, we are running out of effective antibiotics to combat infections.
Efforts to address this issue include promoting responsible antibiotic use, developing new antibiotics, and implementing infection control measures in healthcare settings. Surveillance systems play a crucial role in monitoring the spread of multidrug-resistant bacteria and guiding appropriate treatment strategies.
Researchers and healthcare providers must work together to stay ahead of the evolving threat of antimicrobial resistance. This requires investments in research, education, and policy initiatives to ensure the continued effectiveness of antibiotics for future generations.
It is essential for governments, healthcare organizations, and the pharmaceutical industry to collaborate in developing new strategies to combat antimicrobial resistance. By working together, we can slow down the spread of multidrug-resistant bacteria and protect the health of individuals around the world.
As we continue to face the challenges of antimicrobial resistance, it is crucial to prioritize the development of new treatment options and strengthen global efforts to prevent the spread of resistant bacteria. By taking decisive action now, we can safeguard the effectiveness of antibiotics and protect public health for years to come.
The COVID-19 pandemic has not only brought about the challenge of controlling the spread of the virus, but it has also led to an increase in antibiotic-resistant bacteria, posing a serious threat to public health. A recent study conducted by researchers from the University of São Paulo (ICB-USP) in Brazil has shed light on the rapid growth of multidrug-resistant bacteria, particularly Klebsiella pneumoniae, in Latin America and the Caribbean during the pandemic.
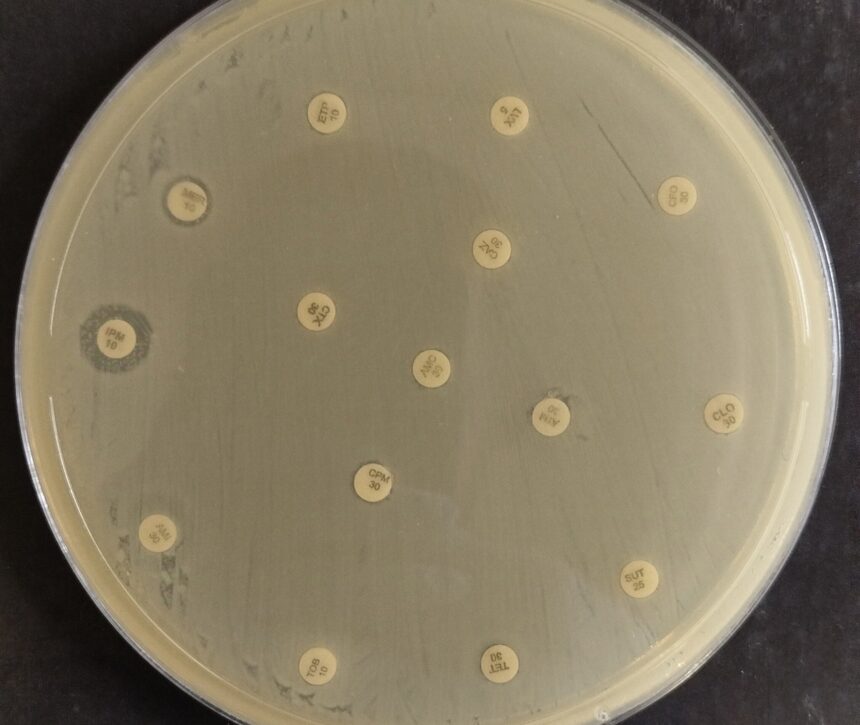
K. pneumoniae is a common cause of hospital-acquired infections, and the emergence of pan-beta-lactam-resistant strains co-producing carbapenemases has raised concerns among health authorities. Carbapenemases are enzymes that render most antibiotics ineffective, making treatment options limited for patients infected with these resistant strains.
Lead researcher Fábio Sellera and his team at UNIMES in Brazil conducted a global genomic analysis, which revealed a significant increase in the prevalence of K. pneumoniae strains resistant to multiple antibiotics. This novel resistance trend poses a serious public health threat and has prompted the Pan American Health Organization (PAHO) and the World Health Organization (WHO) to issue an epidemiological alert.
In response to the growing threat of antibiotic resistance, the FDA approved a new antibiotic, ceftazidime/avibactam, in 2015 for the treatment of K. pneumoniae carbapenemase (KPC)-producing bacteria. However, the rapid evolution of these strains has led to the emergence of bacteria resistant to this latest therapeutic option, leaving patients with few effective treatment options.
Dr. Lincopan, a researcher at ICB-USP, emphasized the importance of monitoring pathogenic bacteria in hospitals and rational prescribing of antibiotics to prevent the spread of drug-resistant strains. Patients are also advised to complete the full course of antibiotic treatment, even if they start feeling better, to prevent the development of resistance.
The study, led by Ph.D. candidate Felipe Vásquez Ponce, highlights the urgent need for continued surveillance and research to combat the rise of antibiotic-resistant bacteria, particularly in the midst of the COVID-19 pandemic. Without effective treatment options and with compromised immune systems, patients infected with these resistant strains face a grim prognosis.