Parkinson’s Disease: Could it Start in the Kidneys?
Parkinson’s disease has long been linked to neurological damage in the brain due to a decrease in dopamine production. However, a recent study suggests a new perspective – the disease may actually originate in an unexpected part of the body: the kidneys.
Conducted by a team from Wuhan University in China, the study focuses on the alpha-synuclein (α-Syn) protein, known for its association with Parkinson’s. When this protein misfolds and forms clumps, it disrupts brain function.
The groundbreaking discovery is that α-Syn clumps can accumulate not only in the brain but also in the kidneys. The researchers propose that these abnormal proteins could potentially travel from the kidneys to the brain, potentially triggering the onset of Parkinson’s disease.
“We demonstrate that the kidney is a peripheral organ that serves as an origin of pathological α-Syn,” stated the researchers in their published paper.
The study involved various tests, including observing α-Syn behavior in genetically modified mice and analyzing human tissue samples, including those from individuals with Parkinson’s disease and chronic kidney disease.
The researchers identified abnormal α-Syn accumulation in the kidneys of 10 out of 11 individuals with Parkinson’s and other forms of dementia associated with Lewy bodies, a common type of α-Syn clumping.
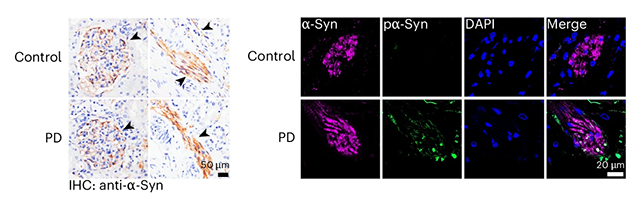
In another set of samples, similar protein abnormalities were found in 17 out of 20 patients with chronic kidney disease, despite the absence of neurological symptoms. This suggests that the kidneys may serve as the initial site for the aggregation of these harmful proteins before the onset of brain damage.
Animal experiments supported these findings. Mice with healthy kidneys efficiently cleared injected α-Syn clumps, whereas mice with impaired kidney function showed protein buildup that eventually spread to the brain. When the neural connection between the brain and kidneys was severed in further tests, this spread did not occur.
Since α-Syn proteins can travel through the bloodstream, the researchers also investigated this pathway. They observed that lower levels of α-Syn in the blood correlated with reduced brain damage, highlighting another potential avenue for intervention.
While the study has some limitations, such as a small sample size of human tissue and the variability between animal models and humans, it presents intriguing findings that warrant further exploration. These discoveries could ultimately contribute to the development of novel therapies for Parkinson’s and related neurological disorders.
It is likely that Parkinson’s, like Alzheimer’s disease, may have multiple triggers and risk factors. Previous research has hinted at potential links to the gut, and now the kidneys emerge as another potential player in the disease’s pathogenesis.
“Removal of α-Syn from the blood may impede the progression of Parkinson’s disease, offering new therapeutic strategies for managing Lewy body diseases,” concluded the researchers.
The study has been published in Nature Neuroscience.





