New Study Challenges Understanding of Prions in Neurodegenerative Diseases
A recent study in mice has raised questions about the traditional understanding of prions and their role in neurodegenerative diseases. Prions are misfolded proteins that are known to cause conditions such as mad cow disease, chronic wasting disease, and Creutzfeldt-Jakob disease. However, the new research suggests that some of the hallmarks of prion disease can develop even in the absence of infectious prions.
The study, led by immunologist Burim Ametaj of the University of Alberta in Canada, found that non-infectious prion precursors, combined with chronic inflammation driven by a bacterial endotoxin, were enough to trigger prion-like neurodegeneration in mice. This challenges the prevailing theory that prion diseases are solely caused by misfolded proteins.
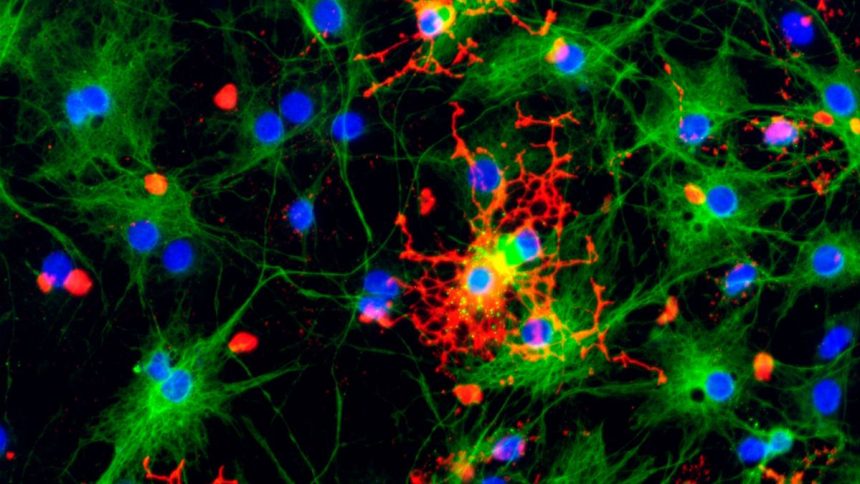
The researchers artificially generated a toxic, misfolded form of a prion protein that is not infectious and administered it to mice. They also gave some mice the bacterial endotoxin lipopolysaccharide (LPS) to induce inflammation. The results showed that mice exposed to non-infectious prions alone developed spongiform brain damage and scarring, while those exposed to LPS alone developed amyloid plaques and spongiform damage.
Combining the non-infectious prions with LPS led to accelerated disease progression, with all mice in this group dying within 200 days. This suggests that inflammation may play a crucial role in the development of neurodegenerative diseases, potentially even before the misfolding of prion proteins occurs.
The findings have important implications for understanding and treating prion diseases, as well as other neurodegenerative conditions like Alzheimer’s, Parkinson’s, and ALS. By targeting inflammation, researchers may be able to develop new therapeutic strategies to combat these devastating diseases.
Overall, this study highlights the complexity of neurodegenerative diseases and the need for further research to uncover the underlying mechanisms. By challenging existing assumptions about prions and inflammation, scientists may be able to develop more effective treatments for these debilitating conditions. Bacterial endotoxins have been discovered in the brains of individuals with Alzheimer’s disease, suggesting a potential link between endotoxin exposure and the development of neurodegenerative disorders. According to Ametaj, risk factors that can reduce the risk of dementia, such as regular exercise, anti-inflammatory diets, maintaining gut health, and metabolic health, may work in part by lowering the burden of endotoxins in the body.
The presence of endotoxins in the brain raises the possibility that managing this modifiable risk factor could potentially prevent a significant proportion of neurodegenerative diseases. Even if endotoxin exposure only contributes to 20-30% of cases, addressing this risk factor could have a significant impact on millions of individuals. By focusing on controlling inflammatory risk factors throughout life, similar to how we approach preventing heart disease, it may be possible to reduce the incidence of neurodegenerative disorders.
The implications of this research are significant, offering hope in a field where treatment options have been limited. The findings have been published in the International Journal of Molecular Sciences, shedding light on a potential new avenue for understanding and potentially addressing neurodegenerative diseases. This new research highlights the importance of considering endotoxin exposure as a potential factor in the development of Alzheimer’s and other related conditions.
Moving forward, further studies will be needed to fully understand the role of bacterial endotoxins in neurodegenerative diseases and to explore potential interventions that could help reduce endotoxin burden in individuals at risk. By continuing to investigate this link and its implications, researchers may uncover new strategies for preventing and managing neurodegenerative disorders in the future.