Tom McAndrew, a computational scientist and associate professor at Lehigh University’s College of Health, recently conducted a study published in The Lancet Digital Health. The study focused on the impact of limiting public health data on researchers and healthcare providers during the influenza season.
During the peak flu season, Pennsylvania typically sees around 1,000 hospitalizations per week. However, last year’s flu season saw a significant increase, with about 4,000 hospitalizations per week, marking one of the worst flu seasons in the U.S. in over a decade.
The challenges arose when President Donald Trump signed executive orders that restricted public health entities, including the U.S. Department of Health and Human Services and the Centers for Disease Control and Prevention (CDC), from releasing essential public health data. This limitation affected crucial information needed for accurate decision-making by doctors and researchers.
The executive orders led to the removal of over 8,000 web pages from various government websites, including vital information on vaccines, veterans’ care, hate crimes, and scientific research. Moreover, routine CDC data sources, such as the “Morbidity and Mortality Weekly Report,” were delayed, impacting flu forecasting efforts.
McAndrew, who has been involved in flu forecasting for seven years, expressed concerns about the uncertainty caused by the government’s actions. He highlighted the importance of transparent and accessible datasets for informed public health decision-making.
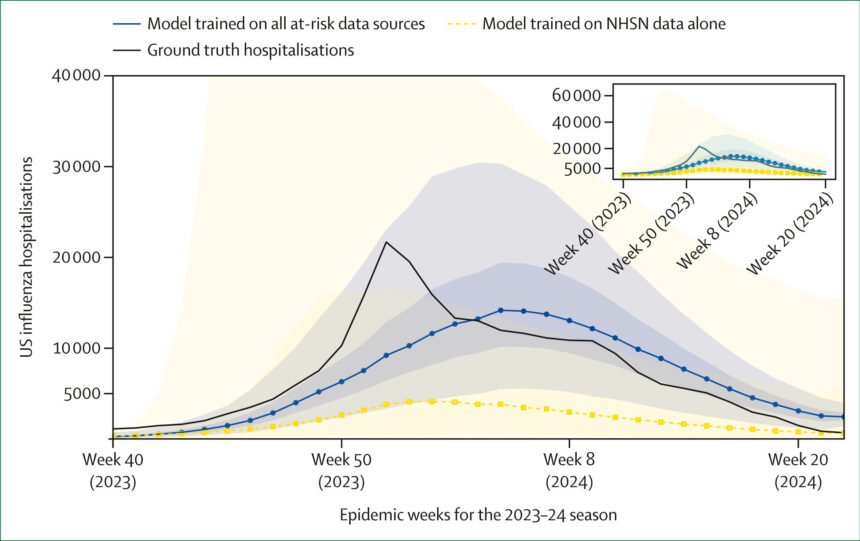
In a collaborative effort with doctoral student Garrik Hoyt, McAndrew published a paper titled “When data disappear: Public health pays as US policy strays” in The Lancet Digital Health. The study demonstrated how the reduction of public health datasets hinders the ability to forecast flu-related hospitalizations and emphasized the risks associated with limiting data access during public health crises.
The researchers compared a data-rich model, incorporating information from seven government sources, with a data-poor model. The findings revealed that the data-rich model produced reliable forecasts crucial for public health decision-making, while the data-poor model resulted in highly uncertain predictions.
The study called for a strategic national plan to safeguard public health data, involving stakeholders from academia, industry, and local government. The goal is to ensure local control over government-hosted datasets, promoting transparent analysis and better public health decision-making.
With the potential consequences of restricted data access on public health, including the current outbreak of avian flu, the researchers emphasized the urgency of protecting and maintaining essential datasets for effective disease surveillance and response.
Hoyt, inspired by personal connections to the impact of flu on vulnerable populations, is working on a follow-up paper that explores the effects of reducing the number of public health officials. The study aims to underscore the value of expert opinions in public health decision-making and highlight the risks associated with diminishing expertise.
Overall, the research conducted by McAndrew, Hoyt, and their team underscores the critical role of data transparency and expert insights in shaping effective public health strategies. As the landscape of public health data continues to evolve, the need for robust data collection and analysis remains essential for safeguarding community health and well-being.