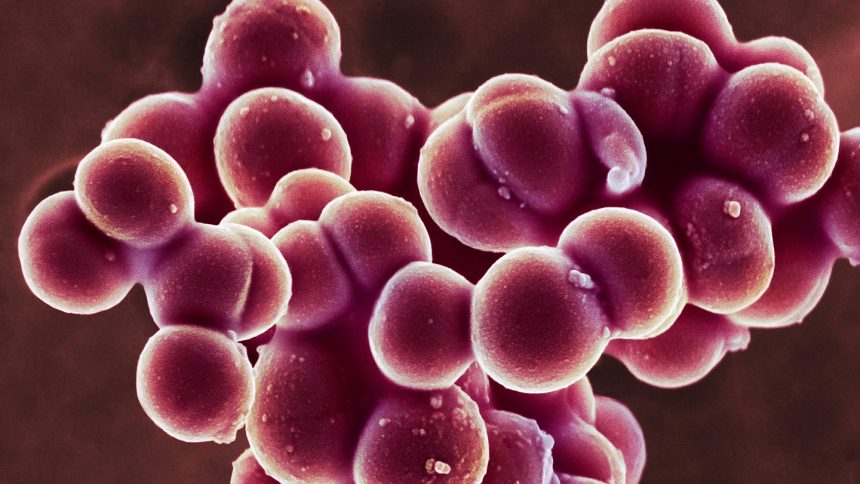
The Sticky Secrets of Staphylococcus aureus: Understanding Its Stronghold on Human Skin
Some microbes possess an uncanny ability to adhere to surfaces, but few are as sticky as Staphylococcus aureus. Known for causing staph infections, this bacterium utilizes “one of the strongest biological bonds ever recorded,” according to a study published in the September 5 issue of Science Advances. This remarkable adhesion is significantly enhanced by the presence of calcium, making it extremely difficult to dislodge the bacteria from human skin.
Calcium’s Double-Edged Sword
Rafael Bernardi, a biophysicist at Auburn University, notes that an influx of calcium can prompt the body to expedite skin healing, particularly in the context of wounds or conditions like eczema. “It’s like a biological boost for your skin,” he explains. However, this same process inadvertently facilitates the bacterial grip, allowing S. aureus to hold on even more tightly when skin is compromised.
As a prevalent skin microbe, S. aureus can infiltrate the body through abrasions, leading to localized skin conditions such as cellulitis, or even serious systemic infections when the bacteria disseminate to other organs. Disrupting the formidable bond between the bacteria and skin could provide valuable insights for developing innovative treatment strategies.
Unpacking the Bond: SdrD and DSG-1
In their research, Bernardi and his team employed microscopy and computer simulations to explore the interaction between the bacterial protein SdrD and the human protein DSG-1 in laboratory settings. They found that in the presence of calcium, these proteins can withstand forces exceeding 2 nanonewtons—an unprecedented strength for a biological bond that doesn’t involve covalent connections, where atoms share electrons.
Most mechanical forces within cells tend to be weaker, typically ranging up to dozens of piconewtons; for instance, it takes around 60 to 80 piconewtons to disrupt the proteins that facilitate muscle contraction. However, the adhesion of SdrD and DSG-1 is approximately 20 times more robust, asserting that at the molecular scale, bacteria like S. aureus can grip surfaces with greater force than the lifting capacity of human muscles, according to Bernardi.
Implications for Clinical Treatment
Individuals often harbor various strains of S. aureus on their skin, but it remains uncertain whether there are differences in binding strength across different strains. Nonetheless, inhibiting the connection between SdrD and DSG-1 could offer a strategic advantage in combating staph infections.
Moreover, certain antibiotic-resistant strains, such as methicillin-resistant S. aureus (MRSA), are known to produce biofilms—slimy protective layers that cluster around bacteria, increasing infection resilience. If bacterial cells cannot attach to the skin effectively, Bernardi suggests, the formation of biofilms is hindered. This opens the door for immune responses or antibiotics to tackle the threat more efficiently.
In summary, understanding the mechanics behind S. aureus‘s adhesion could pave the way for novel therapeutic approaches aimed at preventing bacterial infections, particularly in vulnerable populations. By breaking down this formidable bond, researchers may not only enhance existing treatments but also develop new strategies to effectively manage staph infections.
This article retains the HTML formatting required for a WordPress platform while presenting the content in a unique and informative manner focused on the topic of Staphylococcus aureus and its interactions with human skin.