Researchers at UT Southwestern Medical Center have made a groundbreaking discovery regarding sex-specific differences in the accumulation of fat in muscle and bone. This research could potentially lead to new treatment approaches for age-related diseases, shedding light on how fat infiltrates different tissues in the body.
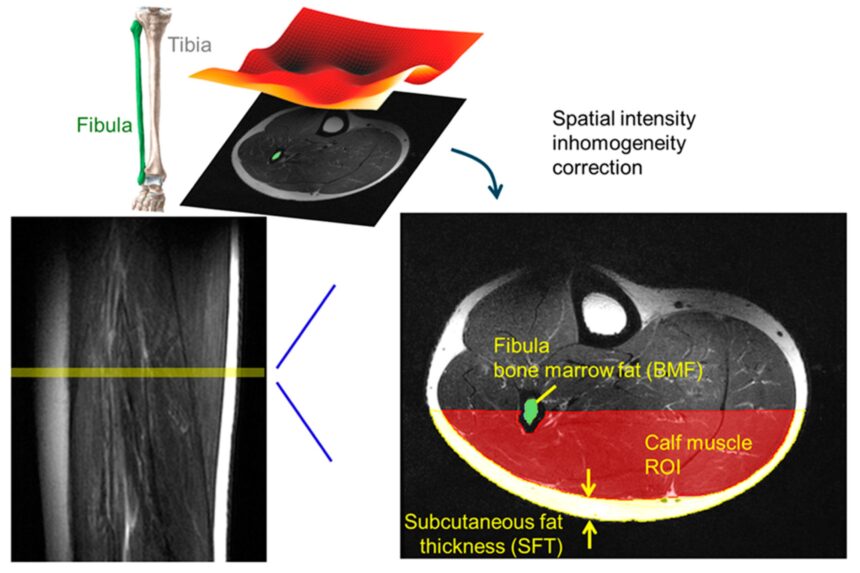
Published in Diagnostics, the study focused on how fat infiltrates skeletal muscle and accumulates in subcutaneous tissue and bone marrow. The findings highlighted key distinctions between men and women, influenced by age and body mass index (BMI). This research is crucial in understanding musculoskeletal disorders, which are a leading cause of disability in the United States.
The study analyzed MRI scans from 107 patients at UT Southwestern, with a diverse demographic range in terms of age, gender, and BMI. The research specifically looked at the lower extremities, revealing that fat infiltration in muscle increased significantly with age in women, while being more closely correlated with body weight in men. Additionally, women had double the average subcutaneous fat thickness compared to men, with this fat increasing with age in women but decreasing in men, especially those who were not obese.
Moreover, the researchers discovered a relationship between muscle fat infiltration and bone marrow cross-sectional area, emphasizing the interconnectedness of muscle and skeletal health. Weak bone structure can facilitate fat infiltration into surrounding muscles, leading to increased risks of falls, fractures, and metabolic disorders. Maintaining overall musculoskeletal strength is crucial for managing age-related conditions, especially in older adults.
Dr. Jimin Ren, the senior author of the study, highlighted the importance of understanding the impact of fat accumulation in muscle on glucose metabolism and overall health. The research also shed light on sex-specific health challenges as individuals age, with hormonal changes in women post-menopause increasing the risk of conditions like sarcopenia and osteoporosis. In men, the study emphasized the significance of managing obesity to protect muscle function.
The findings offer valuable insights for developing personalized strategies to promote musculoskeletal health and prevent age-related decline. By understanding how sex, age, and BMI influence fat distribution in the body, healthcare professionals can tailor exercise regimens, nutrition plans, and therapies to support overall health. Additionally, the research highlights markers that could be used to screen and monitor muscle metabolic health, providing a non-invasive way to assess the risk of conditions like sarcopenia and osteoporosis.
Lead author Dr. Talon Johnson, a postdoctoral research fellow at UT Southwestern, emphasized the potential for dual-targeted therapies that address both muscle and bone health. This integrated approach could pave the way for early interventions in metabolic and musculoskeletal disorders that become more prevalent with age.
In conclusion, this study contributes significantly to our understanding of how sex and age influence fat distribution in muscles and bones. The research opens up new possibilities for personalized care and targeted treatments to support musculoskeletal health and combat age-related conditions.