Growing up in Mbare, the oldest high-density neighborhood in Harare, Zimbabwe, I was only five years old when I first became aware of the unspoken shadow that hung between my mother and me. Tracing the fabric of her gumbezi as sunlight filtered through the room, I had yet to grasp the concept of AIDS. It was a silence that defined my childhood, punctuated by the premature deaths of both my parents before they reached the age of 40, their lives cut short by a virus steeped in stigma and secrecy.
However, despite the hardships I faced, I was given a life-changing opportunity to study in the United States on a scholarship. It was there that I delved into HIV research, immersing myself in internships and collaborations with institutions dedicated to combating the epidemic across Africa. My journey led me to Botswana, where I worked alongside clinical trial teams as the antiretroviral drug dolutegravir emerged as a game-changer in HIV treatment, ultimately recommended by the World Health Organization.
As a medical student on the path to becoming an infectious disease doctor, I closely follow the latest advancements in the field. One such breakthrough that has captured my attention is the approval of Yeztugo, the brand name for lenacapavir developed by Gilead Sciences. This revolutionary injection, administered only twice a year, boasts nearly 100% efficacy in preventing HIV based on global Phase 3 trials involving participants from diverse regions worldwide.
The significance of lenacapavir goes beyond mere statistics for me. It represents a beacon of hope for communities like my own, where the accessibility of prevention measures is often a matter of life and death. While Gilead’s commitment to providing royalty-free licenses to generic manufacturers in low- and middle-income countries is commendable, more needs to be done to ensure equitable access globally.
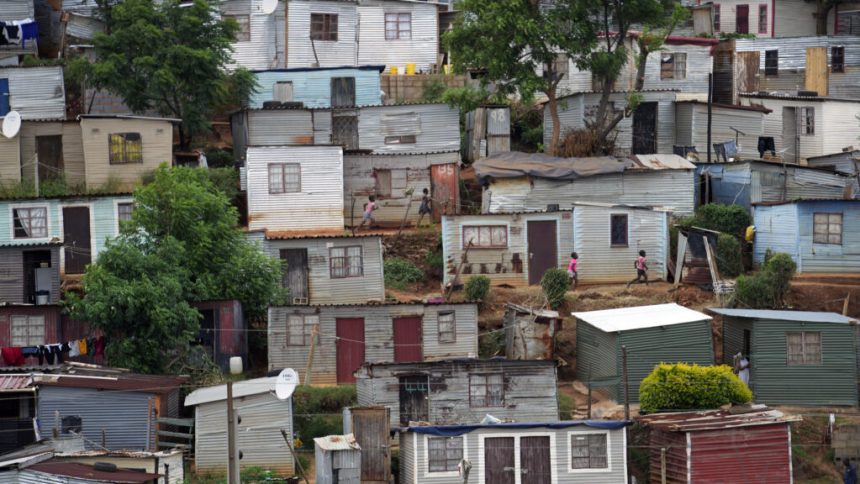
In sub-Saharan Africa, where women and girls bear the brunt of new HIV infections, timely access to preventive medications is critical. Gilead must expand licensing agreements and invest in regional manufacturing to facilitate widespread distribution in partnership with governments and global health organizations. The urgency of the situation demands swift action to prevent needless infections and loss of life.
As I reflect on the disparities in healthcare access that continue to plague vulnerable populations, I am reminded of the young women I have encountered in clinics across Southern Africa. Their skepticism and weariness stem from years of broken promises and missed opportunities for progress. As a future physician, I carry their stories with me, determined to advocate for a more just and inclusive healthcare system that prioritizes the needs of those most affected by the HIV epidemic.
In closing, I urge Gilead and other stakeholders to seize this moment to ensure that lenacapavir and future innovations in HIV prevention are made available to all who need them. This breakthrough belongs to the patients, families, and communities who have borne the burden of the disease for far too long. It is time to turn the tide and make progress a reality for all.