Sexually transmitted infections (STIs) continue to be a prevalent concern in the emergency department, where clinicians often face the dilemma of whether to administer antibiotics preemptively or wait for lab results. A recent systematic review published in Academic Emergency Medicine sheds light on the hidden problem of overtreating men and undertreating women in STI care within emergency departments across the United States.
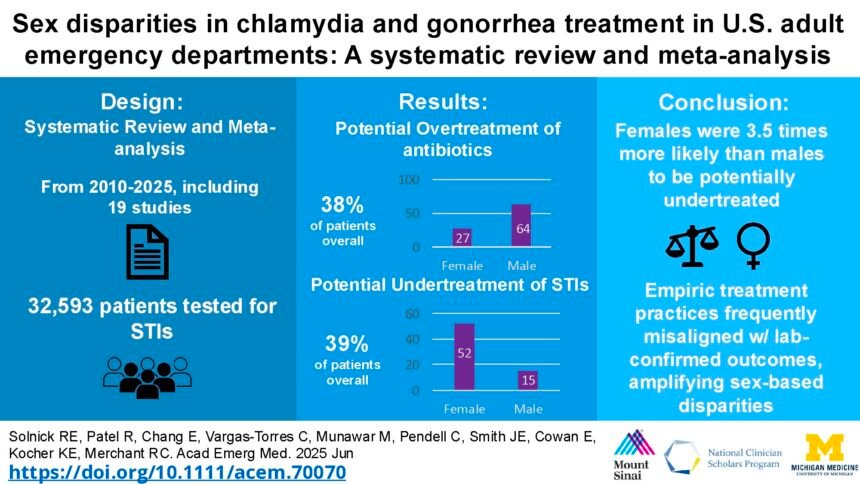
The review uncovered that a significant 38% of ED patients who tested negative for chlamydia or gonorrhea still received antibiotics. This overtreatment not only contributes to antibiotic resistance but also poses risks of unnecessary side effects and inflated medical costs. On the other hand, women were found to be 3.5 times more likely than men to go undertreated for STIs, with more than half of positive cases in women lacking appropriate treatment.
Chlamydia and gonorrhea, if left untreated, can lead to severe consequences such as pelvic inflammatory disease, infertility, and chronic pelvic pain, particularly affecting women. With STI clinics closing and primary care accessibility strained, emergency departments have become crucial hubs for STI diagnosis and treatment. Every decision made in the ED regarding antibiotic administration holds significant weight, as patients may not return for follow-up care.
Among the 32,000 adult ED visits reviewed, 1 in 7 tested positive for chlamydia or gonorrhea, with higher infection rates observed in men compared to women. Nearly half of patients received antibiotics before lab results, leading to potential overtreatment. Furthermore, 39% of positive cases had no record of appropriate treatment, leaving patients at risk of untreated infections.
Factors contributing to these disparities include clear symptoms in men prompting immediate treatment, while women are often tested as part of broader evaluations for non-STI-related complaints, leading to deferred treatment. Additionally, biases in clinical decision-making may result in women being treated less aggressively than men, increasing the likelihood of undertreatment in female patients.
To address these issues, implementing rapid molecular tests for real-time STI detection, engaging in shared decision-making with patients, utilizing ED callbacks for treatment follow-up, and integrating clinical decision support in electronic health records are potential solutions. By recognizing and tracking disparities, adjusting practices based on evidence, and prioritizing equity in STI care, emergency departments can deliver faster, fairer, and more evidence-based care.
In conclusion, addressing the hidden problem of overtreating men and undertreating women in emergency department STI care requires a multifaceted approach that combines advanced diagnostic tools, patient-centered care, and an intentional focus on closing gender gaps in treatment. By optimizing workflows and ensuring equitable care delivery, emergency departments can strive towards providing high-quality STI care that is both efficient and effective.