Lung cancer screening continues to be significantly underutilized, with screening rates as low as 16% according to the American Lung Association. This means that less than 1 in 5 eligible individuals are receiving the low-dose CT scan, which is the recommended screening test for lung cancer. This is concerning as lung cancer is the leading cause of cancer-related deaths among both men and women.
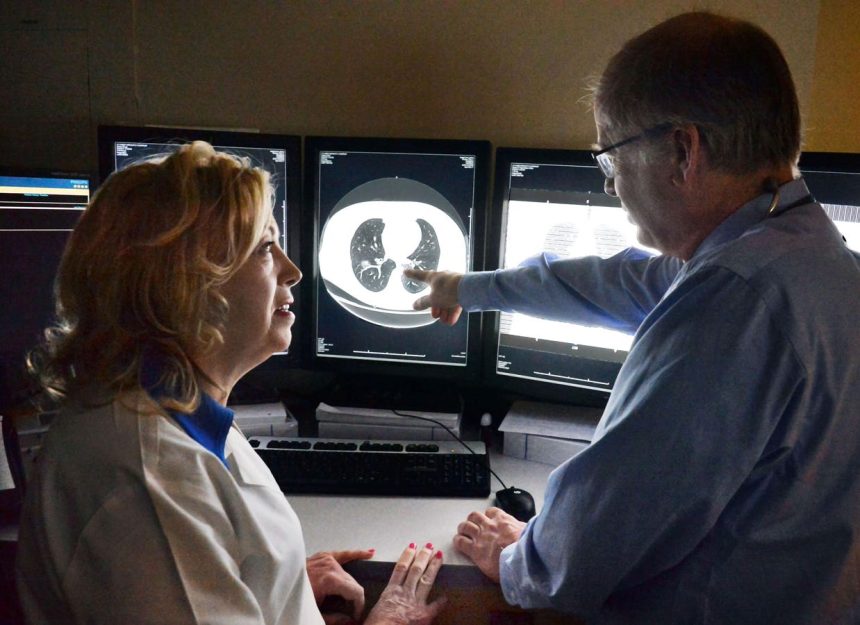
The United States Preventive Services Task Force recommends annual screening for individuals between the ages of 50-80 who have a 20 or more pack-year history of smoking and currently smoke or have quit within the last 15 years. The low dose CT scan takes less than five minutes to perform and has been shown to reduce mortality by 20%. Despite its proven benefits, screening rates remain disappointingly low.
One of the main reasons for low screening rates is a lack of awareness among patients. Many smokers or eligible individuals are unaware of the existence of lung cancer screening or do not understand what the low dose CT scan entails. Fear of a cancer diagnosis, stigma associated with being labeled a smoker, and concerns about radiation exposure from the CT scan are also barriers to screening. However, the amount of radiation from the scan is minimal and comparable to background radiation exposure over six months.
Primary care physicians play a crucial role in discussing the importance of screening tests with patients. However, research shows that less than 10% of physicians regularly discuss lung cancer screening with their patients. Some physicians cite uncertainty about eligibility criteria, managing incidental findings, and lack of time for shared decision-making as reasons for not discussing screening. Additionally, prior authorizations and copays from insurance providers can deter both physicians and patients from pursuing screening.
The recent cancellation of the USPSTF meeting in November raises concerns about delayed guideline updates and unclear public health messaging. This could lead to uncertainty about which tests will be covered by insurance companies, potentially resulting in fewer individuals getting screened for lung cancer.
It is evident that lung cancer screening saves lives. Consistent guidance from the USPSTF and effective communication from physicians are essential to ensure that eligible individuals receive the screening. Educating patients and addressing fear and stigma through community outreach are also crucial in increasing screening rates and improving health outcomes for lung cancer patients.