Cardiac rehabilitation is a crucial aspect of recovery for individuals who have experienced a heart event. As a clinician and researcher in this field, I have come to understand that the most powerful tool we possess is not a medical instrument, but our ability to listen. Listening to patients’ stories, fears, and hopes after a cardiac event is essential for a holistic understanding of their recovery journey.
While traditional clinical metrics are important, they only provide a partial view of a patient’s experience. Qualitative research plays a vital role in giving patients a voice and uncovering the nuances that quantitative data may overlook. By conducting interviews, focus groups, and surveys, we can gain insights into the anxieties, motivations, and barriers that individuals face in their rehabilitation process.
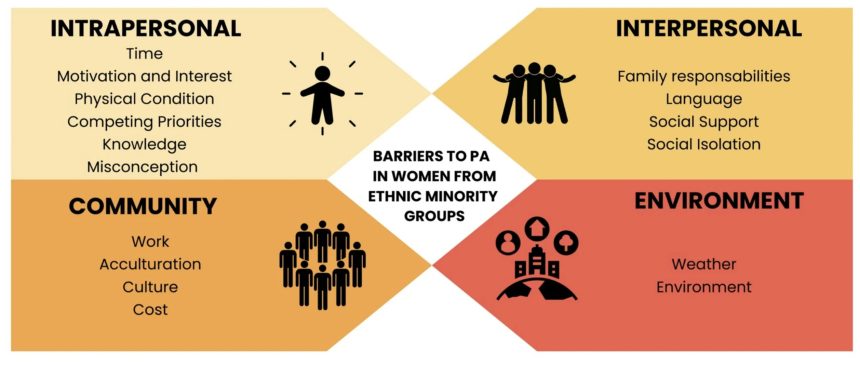
A recent study published in BMC Women’s Health focused on the barriers to physical activity in women from ethnic minority groups. This systematic review highlighted individual, interpersonal, and environmental obstacles to physical activity, such as time constraints, cultural expectations, and unsafe environments. The majority of studies included in the review utilized qualitative methods, emphasizing the importance of listening to the lived experiences of these women to design culturally sensitive interventions.
Incorporating patient perspectives into cardiac rehabilitation programs has been shown to increase engagement, adherence to lifestyle changes, and confidence in managing health. By listening to patients’ stories, clinicians can gain a deeper understanding of the social, cultural, and emotional factors that influence recovery.
What is most striking about these findings is the transformative power of listening. Patient stories contain invaluable insights that can drive innovation in patient education and rehabilitation. By taking the time to truly hear and understand these stories, we can create programs that resonate with patients on a personal level.
Ultimately, cardiac rehabilitation is about more than just physical health—it is about restoring confidence, hope, and a sense of control. Qualitative research serves as a reminder that each individual’s journey to recovery is unique, and effective programs are those that honor and incorporate their experiences.
If we want to truly make a difference in cardiac rehabilitation, we must start by listening. By listening attentively and empathetically to patients’ stories, we can craft narratives that are meaningful and impactful. This approach not only benefits science but, more importantly, the individuals whose lives are touched by cardiac rehabilitation.
In conclusion, the key to telling a good story about cardiac recovery lies in our ability to listen. Only by listening can we create programs that are truly patient-centered and effective in supporting individuals on their path to recovery.