COVID-19 Could Lead to Protein Build-up in Eyes Similar to Alzheimer’s, Study Finds
A recent study suggests that COVID-19 could result in a protein build-up in the eyes, similar to what is seen in Alzheimer’s patients. This discovery may explain why ‘brain fog’, a common symptom of COVID-19, is often reported by patients.
The research, led by Yale University, aimed to investigate the potential connection between COVID brain fog and Alzheimer’s disease. The study explored whether the SARS-CoV-2 virus could lead to the formation of Alzheimer’s-like plaques, which might account for post-infection cognitive issues.
According to senior author Brian Hafler, an ophthalmologist at Yale School of Medicine, “There is mounting evidence linking COVID-19 and brain fog, a prevalent symptom following infection. While the exact mechanisms of brain fog post COVID-19 are not fully understood, researchers have found that SARS-CoV-2 can trigger the accumulation of amyloid beta in the central nervous system.”
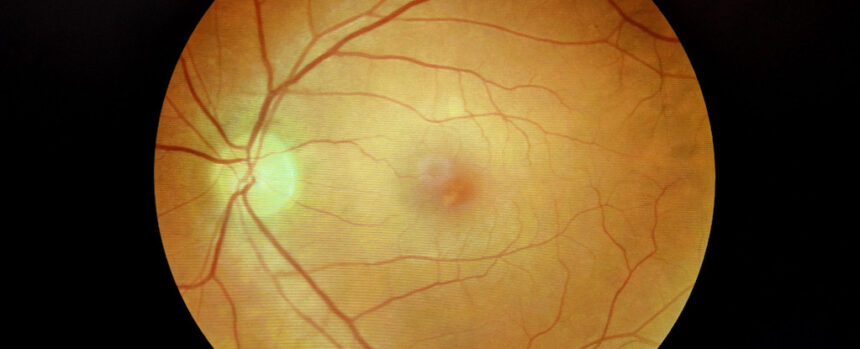
Retinas are considered part of the central nervous system, making them a valuable area for investigation. Previous studies have shown that amyloid beta accumulates in the retinas of Alzheimer’s patients, suggesting that retinal testing could serve as a practical method for diagnosing and monitoring Alzheimer’s disease on a large scale.
In their research, scientists utilized postmortem human retinal tissue and developed retinal organoids – 3D models derived from human stem cells. They analyzed various cell types in the retinal tissue to assess protein production and focused on two proteins, neuropilin-1 (NRP1) and angiotensin-converting enzyme 2 (ACE2), which are potential targets for SARS-CoV-2 to infiltrate neurons.
The study revealed elevated levels of amyloid beta in retinal tissue of individuals with a history of COVID-19, even in those without dementia. Additionally, exposure to SARS-CoV-2 spike protein led to an increase in amyloid beta levels in retinal organoids.
By introducing an NRP1 inhibitor, researchers were able to counter the rise in amyloid beta caused by exposure to the coronavirus spike protein. This suggests that targeting NRP1 could potentially mitigate neurological complications of COVID, including brain fog.
Hafler notes, “Our study demonstrates that exposure to SARS-CoV-2, specifically the spike protein, can result in the formation of amyloid beta aggregates in human retinal tissue and retinal organoids.”
Besides shedding light on COVID-related brain fog, the study supports the idea that amyloid beta may serve as a protective mechanism for the brain. While previously associated with Alzheimer’s pathology, amyloid beta is now viewed as a response to underlying threats.
Further research is needed to explore whether other viruses could trigger similar amyloid beta build-ups. Hafler and his team are currently conducting clinical studies to determine if COVID-19 could heighten the risk of Alzheimer’s disease in the long term.
The ultimate goal of the research is to prevent lasting neurological effects of COVID-19 and investigate potential therapeutics, such as NRP1 inhibitors, to combat viral-induced amyloid pathology and Alzheimer’s disease.
The findings of the study were published in the journal Science Advances.