At the recent Menopause Society annual meeting, researchers revealed new findings that suggest hormone therapy can have a positive impact on the heart health of menopausal women. This therapy was shown to reduce insulin resistance and improve cardiovascular biomarkers, adding to the existing evidence of its benefits in alleviating symptoms like hot flashes, sleep disturbances, vaginal dryness, and pain during intercourse.
Despite the proven advantages of hormone therapy, its usage has significantly declined over the past few decades. In 1999, nearly 27% of menopausal women in the U.S. used estrogen, but by 2020, this number had dropped to less than 5%. Misconceptions about the risks associated with hormone therapy and the societal taboo around discussing menopause have contributed to this underutilization of effective treatments.
The decline in hormone therapy usage can be traced back to a pivotal 2002 study known as the Women’s Health Initiative, which suggested an increased risk of heart disease and breast cancer with the use of estrogen and progestin therapy in older postmenopausal women. However, subsequent research has revealed that the risks associated with hormone therapy for menopausal women, especially those under the age of 60, are relatively low when used to manage symptoms.
Further studies presented at the Menopause Society meeting highlighted the individualized nature of hormone therapy, indicating that age should not be a limiting factor for women in their 70s experiencing persistent hot flashes. The decision to pursue hormone therapy should consider specific risk factors and health status, emphasizing the importance of personalized treatment plans.
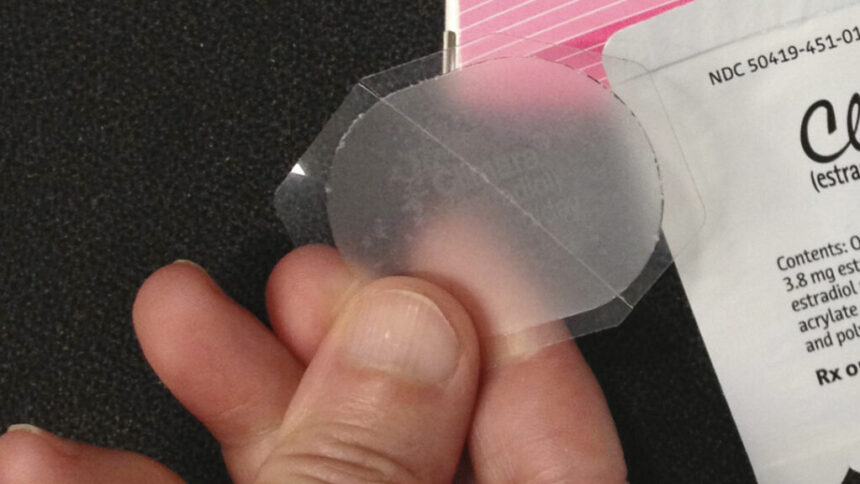
The difference between systemic hormone therapy, which involves a higher dose absorbed into the bloodstream, and local estrogen treatment, which targets vaginal or urinary symptoms with a lower dose, can be confusing for patients. Advocacy groups like Let’s Talk Menopause are pushing for the removal of black box warnings on local estrogen products, citing the lesser risks associated with these treatments compared to systemic estrogen.
Ultimately, the decision to pursue hormone therapy during menopause should be based on an individual’s symptoms, personal philosophy on aging, and risk factors. Healthcare providers, particularly primary care doctors, need to be well-informed about menopause treatment options to guide patients effectively. By promoting awareness of the safety and efficacy of hormone therapy, more menopausal women can benefit from these treatments and improve their quality of life.