An international study published in The Lancet Microbe has shed light on the concerning link between the increased use of disinfectants in intensive care units and the rise of antibiotic-resistant bacteria. The research, led by Professor Marco Oggioni from the University of Bologna, emphasizes the need for a reevaluation of current healthcare guidelines regarding the widespread application of disinfectants.
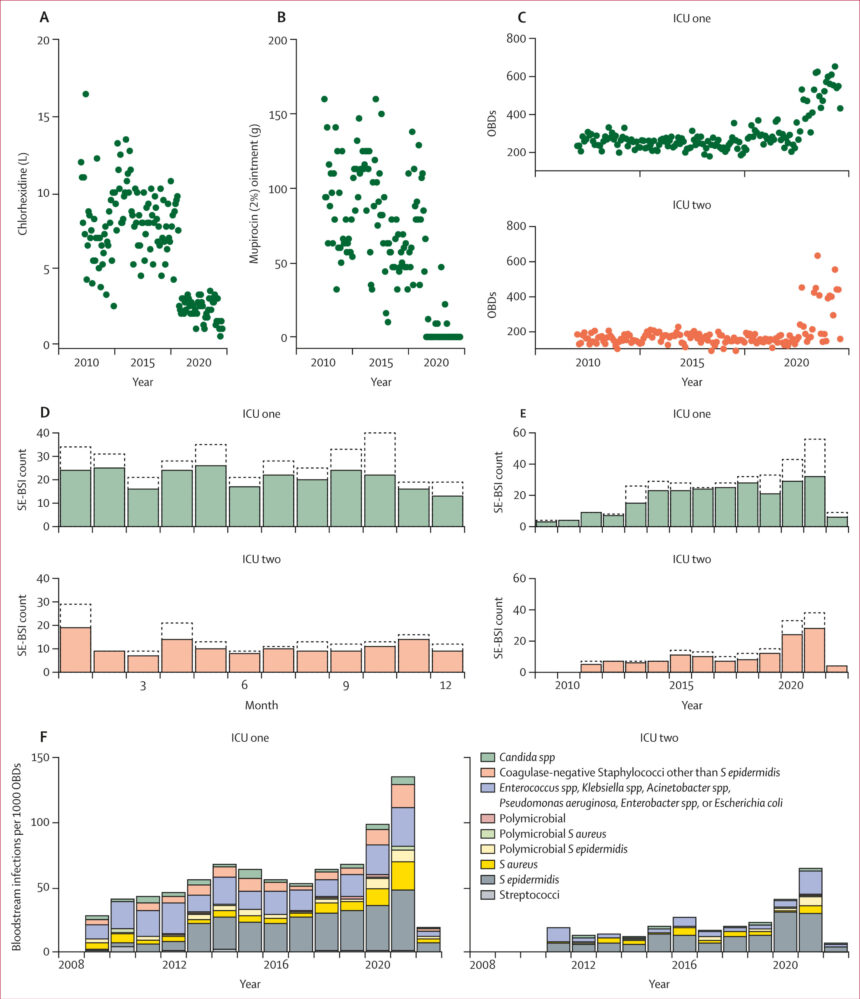
The study focused on universal decolonization procedures, a preventive measure routinely used in intensive care settings. This procedure involves the comprehensive disinfection of patients with chlorhexidine, a common antiseptic, along with nasal treatment using mupirocin. While initially effective in combatting the spread of MRSA (Methicillin-Resistant Staphylococcus aureus), a bacteria resistant to certain antibiotics, the study revealed unintended consequences associated with this approach.
Comparing two hospitals in Scotland with different decolonization strategies, the researchers found higher rates of infections caused by MRSE (Methicillin-Resistant Staphylococcus epidermidis) in the facility practicing universal decolonization. MRSE, although less known than MRSA, is increasingly prevalent and resistant to various antibiotics. This suggests that excessive disinfectant use may not only be ineffective in controlling infections but also contribute to the emergence of antibiotic-resistant strains.
Professor Oggioni underscores the importance of tailored approaches based on regional epidemiological data. While universal decolonization may be necessary in regions with high MRSA prevalence, like Italy, it may be counterproductive in areas with lower infection risks. The study advocates for the development of standardized guidelines that balance the benefits of infection control with the potential impact on antibiotic resistance.
In conclusion, the research calls for a critical reassessment of current practices in light of evolving epidemiological trends. By identifying the most effective decolonization treatments and minimizing the risk of antibiotic resistance, healthcare facilities can better protect patients from infections while mitigating the spread of drug-resistant bacteria.
For more information, the study titled “Universal versus targeted chlorhexidine and mupirocin decolonization and clinical and molecular epidemiology of Staphylococcus epidermidis bloodstream infections in patients in intensive care in Scotland, UK” can be accessed in The Lancet Microbe (2025). DOI: 10.1016/j.lanmic.2025.101118. This research was conducted by the University of Bologna.