A recent study published in The Lancet Global Health has shed light on the significant global and regional disparities in the burden of life-threatening maternal morbidity experienced by women throughout their reproductive years. The research, conducted by experts from the Leverhulme Centre for Demographic Science and London School of Hygiene & Tropical Medicine, is the first of its kind to calculate the lifetime risk of maternal near miss in 40 countries across Asia, Africa, the Middle East, and Latin America from 2010 onwards.
Maternal near miss refers to cases where a woman survives a life-threatening complication during pregnancy or childbirth. These cases are identified by the World Health Organization using specific clinical, laboratory, and intervention-based criteria. The study provides a comparison of the likelihood that a woman aged 15 will experience a maternal near miss before the age of 50, based on the prevalence of such cases, fertility rates, and mortality levels in each country.
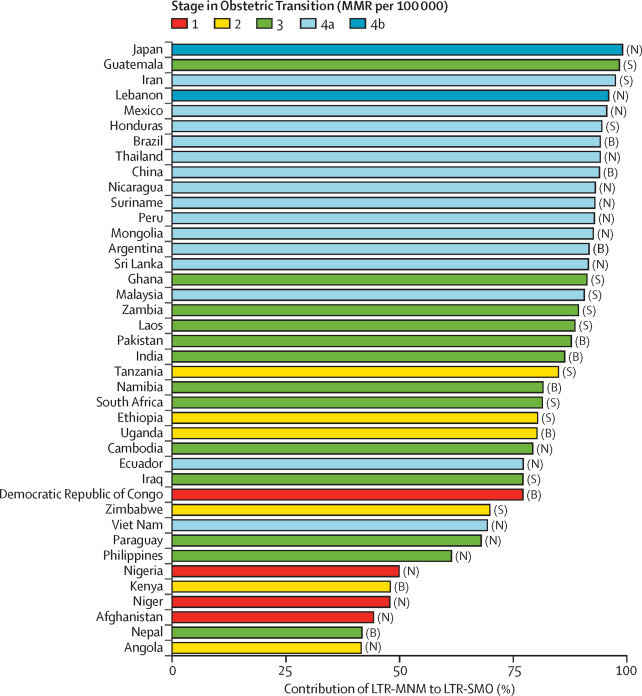
The findings reveal that the lifetime risk of maternal near miss is one in 20 or higher in nine countries, with seven of them located in sub-Saharan Africa. The highest risk was found in Guatemala, where the likelihood is one in six, while the lowest risk was in Vietnam, with a risk of one in 269. These disparities are influenced by obstetric risk levels, fertility rates, and survival rates during reproductive ages.
Lead author Ursula Gazeley emphasized the need to address these inequalities, stating that the study highlights the urgent need for global efforts to improve maternal outcomes. The impact of surviving a life-threatening complication can have long-term effects on a woman’s physical, psychological, social, and economic well-being.
The study also revealed significant variations in the lifetime risk of severe maternal outcomes, with some countries showing a risk as high as one in five. Dr. José Manuel Aburto, one of the researchers, stressed the importance of addressing these challenges to prevent unnecessary maternal morbidity and mortality.
To improve data collection and monitoring of maternal near miss cases, the study recommends applying standardized criteria across different income settings. Establishing surveillance systems to track maternal near miss complications at a national level is crucial for enhancing the availability of data and ensuring better maternal health outcomes globally.
In conclusion, the study serves as a call to action for the global community to prioritize maternal health and work towards reducing the burden of maternal morbidity and mortality. By addressing these disparities and implementing effective interventions, we can strive towards a future where every woman has access to safe and quality maternal care.