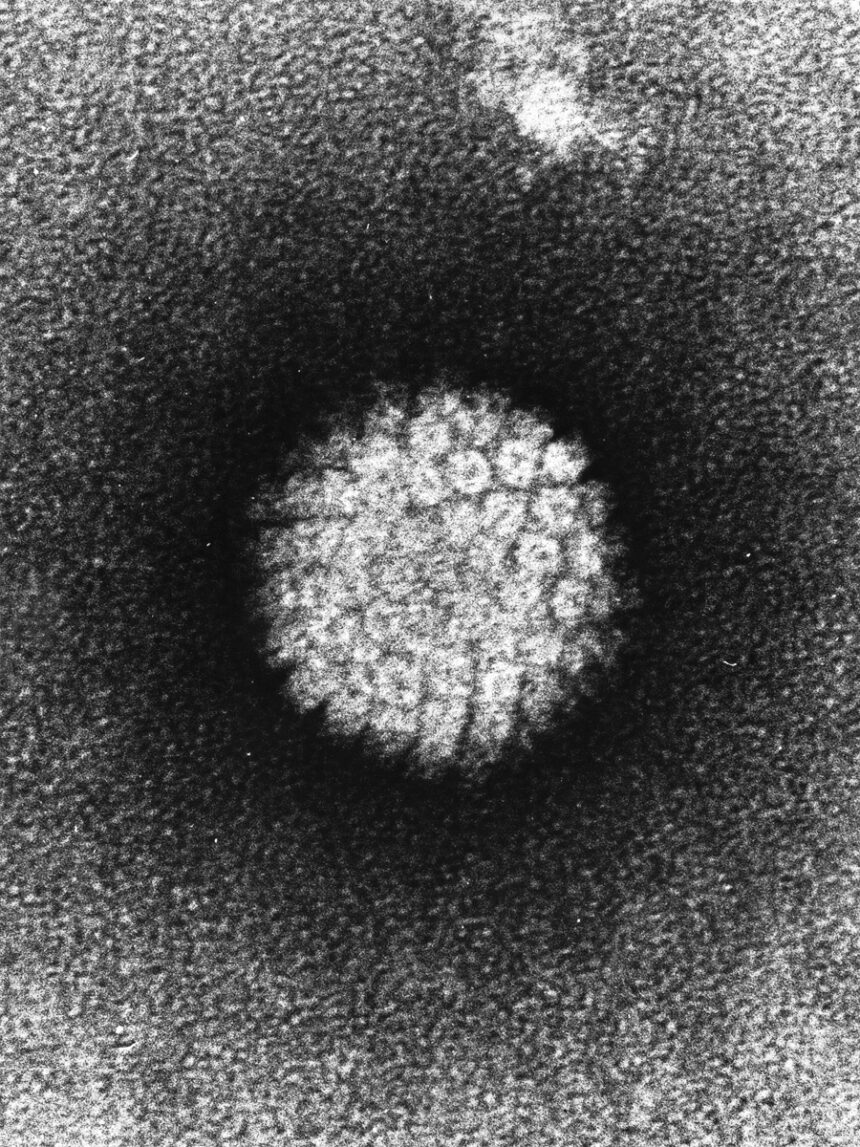
The University of Michigan researchers have conducted groundbreaking studies that demonstrate the effectiveness of self-sampling for HPV detection in the United States. Genital human papillomavirus (HPV) is the most common sexually transmitted infection in the country and is a major risk factor for cervical cancer. Screening for HPV usually involves a speculum-based exam, which can be uncomfortable and inconvenient for many patients, especially those with physical disabilities.
In the two studies published in Preventive Medicine Reports and JAMA Network Open, the researchers found that self-sampling is just as effective as speculum-based testing for HPV detection. Most people infected with HPV are unaware of their infection, and by age 50, the majority of women have been infected with the virus at some point in their lives. While most infections clear up on their own, some can persist and increase the risk of cervical cancer.
Currently, cervical cancer screening and HPV testing are recommended for women every 3 to 5 years starting at age 25. The researchers found that co-testing for HPV and cervical cancer is not significantly more beneficial than testing for HPV alone. This new method of self-sampling not only improves the overall screening experience but also reduces the physical and emotional toll on patients.
The study involved a cohort of 193 individuals aged 25 to 65 who underwent routine screening or were at risk for cervical cancer. The participants used vaginal swabs for self-sampling, which were then collected and sent to the laboratory for testing. The results showed that self-sampling with vaginal swabs was equivalent to speculum-based collection in detecting high-risk HPV types.
Furthermore, the researchers also focused on women with physical disabilities who face barriers to traditional cervical cancer screening methods. Using a cohort of 56 women with physical disabilities, the study found that these women preferred self-sampling with vaginal swabs over speculum exams. The at-home self-sampling was described as simple, comfortable, and feasible, compared to the cold, traumatizing, and invasive experience of in-office speculum-based screenings.
The researchers are now working with U-M Health to make self-sampling the primary method for cervical cancer screening in their clinics. They hope that the results from these studies will inform education and promotion efforts for all individuals. This collaborative effort highlights the importance of interdisciplinary research and the potential for self-sampling to revolutionize cervical cancer screening in the United States.
In conclusion, the University of Michigan researchers have made significant strides in improving HPV screening and detection through self-sampling. Their studies have shown that self-sampling with vaginal swabs is just as effective as speculum-based testing and can enhance the screening experience for all individuals, especially those with physical disabilities. This innovative approach has the potential to transform cervical cancer screening practices and reduce the incidence of this deadly disease.